-
Dynamic and precise measurement of cerebral blood flow velocity plays a critical role in neuroscience and the diagnosis of cerebrovascular diseases. Traditional color Doppler ultrasound can only measure the velocity component along the ultrasound beam, thus limiting its ability to accurately capture the full blood flow vector in complex environments. To break through these limitations, we propose an ultrafast pulse-coded vector Doppler (PC-UVD) imaging method, by using Hadamard matrix pulse encoding to enhance velocity estimation accuracy in low signal-to-noise ratio (SNR) conditions. Our study includes spiral flow simulations and in vivo rat brain experiments, which demonstrate significantly improved measurement precision compared with traditional ultrafast vector Doppler (UVD). This novel approach can measure dynamic cerebral blood flow velocity within a single cardiac cycle, presenting insights into cerebrovascular resistivity characteristics. The proposed PC-UVD method encodes plane waves with Hadamard matrices and can increase SNR without sacrificing temporal or spatial resolution. Velocity vectors are then estimated using a weighted least squares (WLS) approach, where iterative residual-based weight optimization enhances robustness to noise and reduces contributions of outliers. The effectiveness of this technique is validated through simulations using a spiral blood flow phantom, indicating a substantial improvement in velocity estimation accuracy, especially in deep imaging regions with significant signal attenuation. In vivo experiments on rat brains further corroborate that the proposed method has higher accuracy than existing UVD approaches, especially for small vessels. Notably, our method can accurately distinguish between arterial flow and venous flow by analyzing pulsatility and resistivity within the cerebral vascular network. This work demonstrates the potential of PC-UVD in complex vascular imaging, providing high SNR, high temporal and spatial resolution, and accurate vectorized flow measurements. Our results highlight its ability to non-invasively evaluate hemodynamic parameters and its potential application in the diagnosis of cerebrovascular diseases, particularly in small vessels. -
Keywords:
- vector Doppler imaging /
- blood flow velocity /
- flow resistivity /
- ultrafast ultrasound /
- pulse code
[1] Bandera E, Botteri M, Minelli C, Sutton A, Abrams K R, Latronico N 2006 Stroke 37 1334
 Google Scholar
Google Scholar
[2] Geurts L J, Zwanenburg J J M, Klijn C J M, Luijten P R, Biessels G J 2018 Stroke 50 1
 Google Scholar
Google Scholar
[3] Logothetis N K 2008 Nature 453 869
 Google Scholar
Google Scholar
[4] Salmela M B, Mortazavi S, Jagadeesan B D, Broderick D F, Burns J, Deshmukh T K, Harvey H B, Hoang J, Hunt C H, Kennedy T A, Khalessi A A, Mack W, Patel N D, Perlmutter J S, Policeni B, Schroeder J W, Setzen G, Whitehead M T, Cornelius R S, Corey A S 2017 J. Am. Coll. Radiol. 14 S34
 Google Scholar
Google Scholar
[5] Poelma C 2017 Exp. Fluids 58 1
 Google Scholar
Google Scholar
[6] Poelma C, van der Mijle R M E, Mari J M, Tang M X, Weinberg P D, Westerweel J 2012 Eur. J. Mech. B. Fluids 35 70
 Google Scholar
Google Scholar
[7] Omoto R, Kasai C 1986 Echocardiography 3 463
 Google Scholar
Google Scholar
[8] Kripfgans O D, Rubin J M, Hall A L, Fowlkes J B 2006 Ultrasound Med. Biol. 32 1037
 Google Scholar
Google Scholar
[9] Udesen J, Jensen J A 2006 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 53 959
 Google Scholar
Google Scholar
[10] Bohs L N, Geiman B J, Anderson M E, Gebhart S C, Trahey G E 2000 Ultrasonics 38 369
 Google Scholar
Google Scholar
[11] Fahrbach K 1969 Biomed. Tech. 14 233
 Google Scholar
Google Scholar
[12] Peronneau P, Bournat J, Bugnon A, Barbet A, Xhaard M 1974 Cardiovasc. Appl. Ultrasound 1 66
[13] Wang W Q, Yao L X 1982 Ultrasound Med. Biol. 8 421
 Google Scholar
Google Scholar
[14] Tsang I K H, Yiu B Y S, Yu A C H 2009 IEEE Int. Ultrason. Symp. 2009 1387
 Google Scholar
Google Scholar
[15] Bercoff J, Montaldo G, Loupas T, Savery D, Mézière F, Fink M, Tanter M 2011 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 58 134
 Google Scholar
Google Scholar
[16] Denarie B, Tangen T A, Ekroll I K, Rolim N, Torp H, Bjastad T, Lovstakken L 2013 IEEE Trans. Med. Imaging 32 1265
 Google Scholar
Google Scholar
[17] 臧佳琦, 许凯亮, 韩清见, 陆起涌, 梅永丰, 他得安 2021 70 114304
 Google Scholar
Google Scholar
Zang J Q, Xu K L, Han Q J, Lu Q Y, Mei Y F, Ta D A 2021 Acta Phys. Sin. 70 114304
 Google Scholar
Google Scholar
[18] Demene C, Deffieux T, Pernot M, Osmanski B F, Biran V, Gennisson J L, Sieu L A, Bergel A, Franqui S, Correas J M, Cohen I, Baud O, Tanter M 2015 IEEE Trans. Med. Imaging 34 2271
 Google Scholar
Google Scholar
[19] Sui Y H, Yan S Y, Yu J J, Song J P, Ta D A, Wang W Q, Xu K 2022 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 69 2425
 Google Scholar
Google Scholar
[20] Huang L J, Wang Y D, Wang R, Wei X Y, He Q, Zheng C C, Peng H, Luo J W 2023 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 70 378
 Google Scholar
Google Scholar
[21] Chen Y R, Fang B H, Meng F L, Luo J W, Luo X B 2024 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 71 459
 Google Scholar
Google Scholar
[22] 闫少渊, 许凯亮, 他得安 2023 复旦学报(自然科学版) 62 409
 Google Scholar
Google Scholar
Yan S Y, Xu K L, Ta D A 2023 J. Fudan Univ. (Nat. Sci.) 62 409
 Google Scholar
Google Scholar
[23] Yiu B Y, Yu A C 2016 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 63 1733
 Google Scholar
Google Scholar
[24] 王康宇, 周昱林, 何丽媛, 卢春尧, 于润, 吴大伟 2022 71 104303
 Google Scholar
Google Scholar
Wang K Y, Zhou Y L, He L Y, Lu C Y, Yu R, Wu D W 2022 Acta Phys. Sin. 71 104303
 Google Scholar
Google Scholar
[25] Yan S Y, Shou J J, Yu J J, Song J P, Mao Y, Xu K L 2023 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 70 613
 Google Scholar
Google Scholar
[26] Gong P, Song P F, Chen S G 2017 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 64 1674
 Google Scholar
Google Scholar
[27] Gong P, Song P F, Huang C W, Chen S G 2018 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 65 1977
 Google Scholar
Google Scholar
[28] Ferrara K, DeAngelis G 1997 Ultrasound Med. Biol. 23 321
 Google Scholar
Google Scholar
[29] Demene C, Pernot M, Biran V, Alison M, Fink M, Baud O, Tanter M 2014 J. Cereb. Blood Flow Metab. 34 1009
 Google Scholar
Google Scholar
[30] Jensen J A, Svendsen N B 1992 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 39 262
 Google Scholar
Google Scholar
[31] Jensen J A 1997 Med. Biol. Eng. Comput. 34 351
[32] Rabut C, Correia M, Finel V, Pezet S, Pernot M, Deffieux T, Tanter M 2019 Nat. Methods 16 994
 Google Scholar
Google Scholar
[33] Posada D, Poree J, Pellissier A, Chayer B, Tournoux F, Cloutier G, Garcia D 2016 IEEE Trans. Med. Imaging 35 1510
 Google Scholar
Google Scholar
[34] Poree J, Goudot G, Pedreira O, Laborie E, Khider L, Mirault T, Messas E, Julia P, Alsac J M, Tanter M, Pernot M 2021 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 68 2117
 Google Scholar
Google Scholar
[35] Ecarlat P, Perrot V, Carcreff E, Nicolas B, Liebgott H, Garcia D 2022 IEEE Int. Ultrason. Symp. 2022 1
 Google Scholar
Google Scholar
[36] Nahas H, Au J S, Ishii T, Yiu B Y S, Chee A J Y, Yu A C H 2020 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 67 2615
 Google Scholar
Google Scholar
[37] Nahas H, Ishii T, Yiu B Y S, Yu A C H 2023 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 70 1384
 Google Scholar
Google Scholar
[38] 付亚鹏, 孙乾东, 李博艺, 他得安, 许凯亮 2023 72 074302
 Google Scholar
Google Scholar
Fu Y P, Sun Q D, Li B Y, Ta D A, Xu K L 2023 Acta Phys. Sin. 72 074302
 Google Scholar
Google Scholar
-
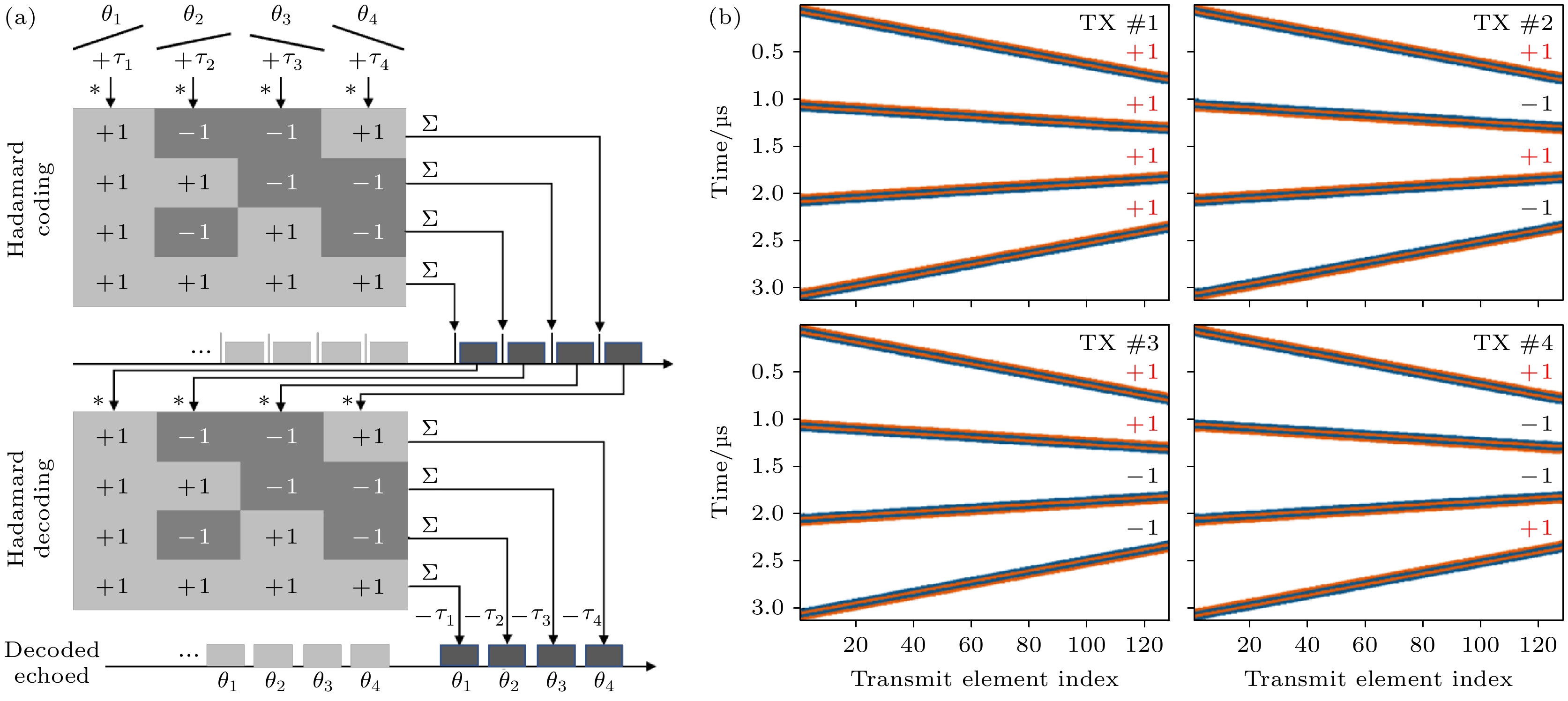
图 1 基于Hadamard编码的多脉冲平面波编码解码方法 (a) 使用4阶Hadamard矩阵对四个平面波进行编码和解码的示意图; (b) 四次发射事件的波形示例
Figure 1. Hadamard-based multiplane wave encoding and decoding: (a) Schematic representation of the encoding and decoding process using a Hadamard matrix for four plane waves; (b) waveform examples for the four transmission events.
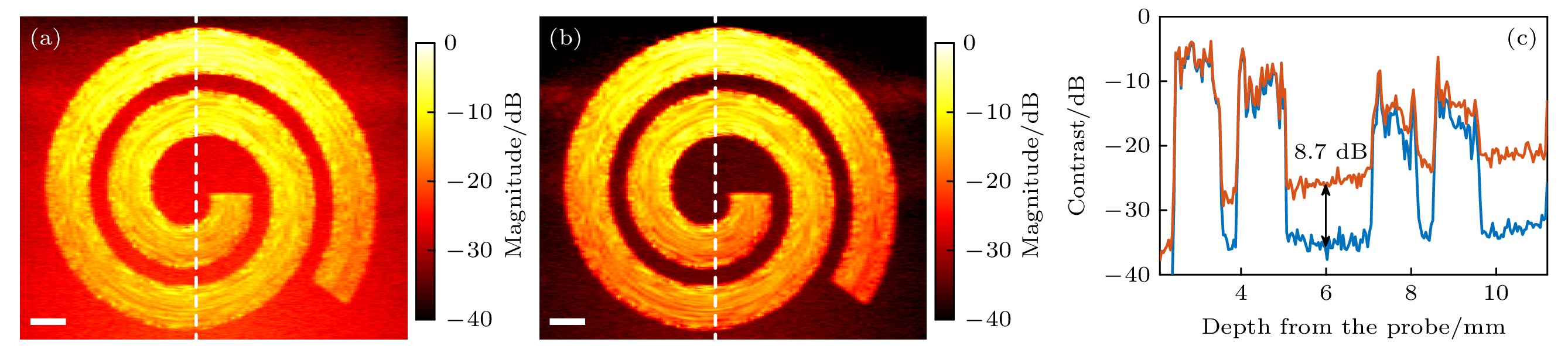
图 2 超快功率多普勒(power Doppler, PD)和超快脉冲编码功率多普勒(PC-PD)螺旋血流仿真成像结果 (a) PD仿真结果; (b) PC-PD仿真结果; (c) SNR量化曲线, 显示了不同深度下的血流与背景噪声信号强度对比
Figure 2. Simulated results of spiral flow power Doppler imaging based on conventional ultrafast ultrasound power Doppler (PD) and pulse coded power Doppler (PC-PD): (a) PD simulation result; (b) PC-PD simulation result; (c) SNR quantization curve, showing the contrast of blood flow and background noise at different depths.
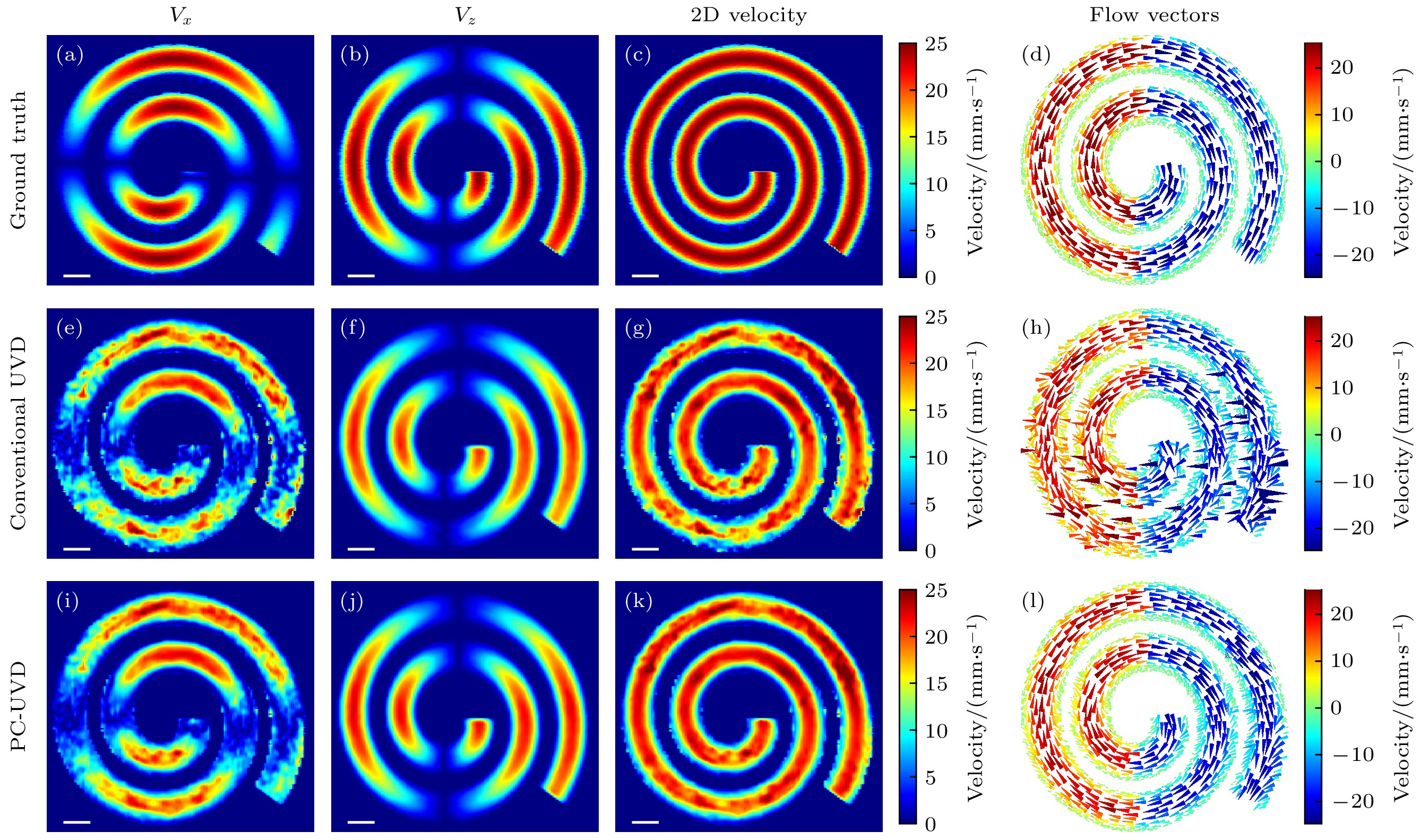
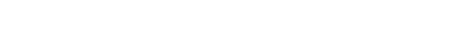
图 3 螺旋血流模型超快矢量多普勒血流速度仿真结果. 从上到下各行分别展示了理论速度真值, 常规UVD和PC-UVD测量得到的血流速度图. 每行分别包含血流速度的水平分量(Vx)、竖直分量(Vz)、二维速度以及矢量化血流成像结果
Figure 3. Simulated results of vector velocity in spiral blood flow, including the ground velocity truth (top row), conventional UVD (middle row), and PC-UVD (bottom row) for blood flow velocity. Each row contains the horizontal velocity component Vx (first column), vertical velocity component Vz (second column), 2D velocity (third column), and vectorized blood flow imaging results (fourth column), respectively.
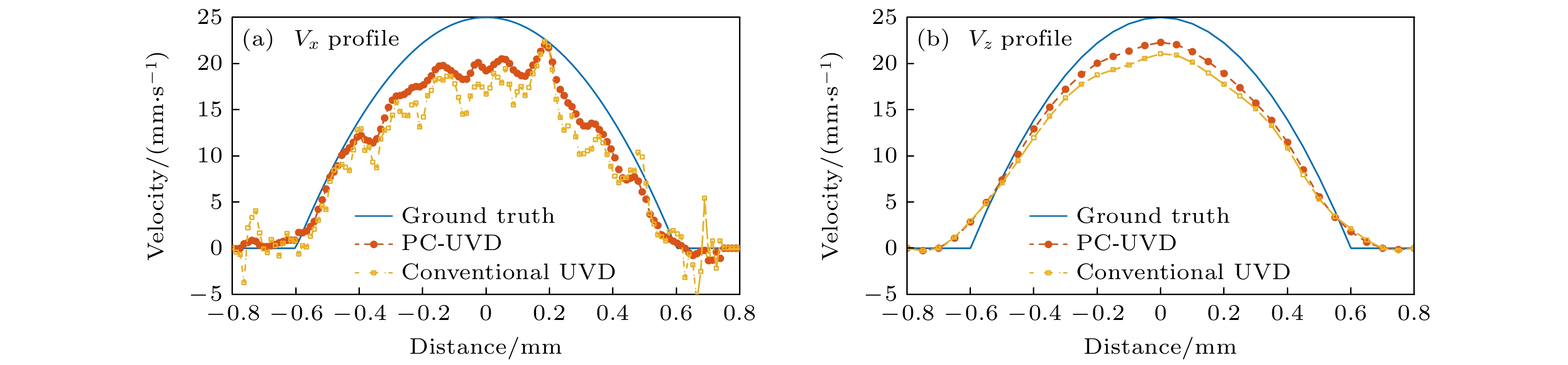
图 4 基于超快矢量多普勒的螺旋血流水平和竖直方向速度剖线 (a)水平速度分布; (b)竖直速度分布. 蓝线表示理论速度分布, 黄线表示常规UVD测量结果, 红线表示PC-UVD测量结果
Figure 4. Horizontal and vertical velocity profiles of spiral blood flow measured by ultrafast vector Doppler: (a) Lateral velocity distribution; (b) axial velocity distribution. The blue line represents the velocity ground truth, the yellow line represents the conventional UVD measurement, and the red line represents the PC-UVD measurement.
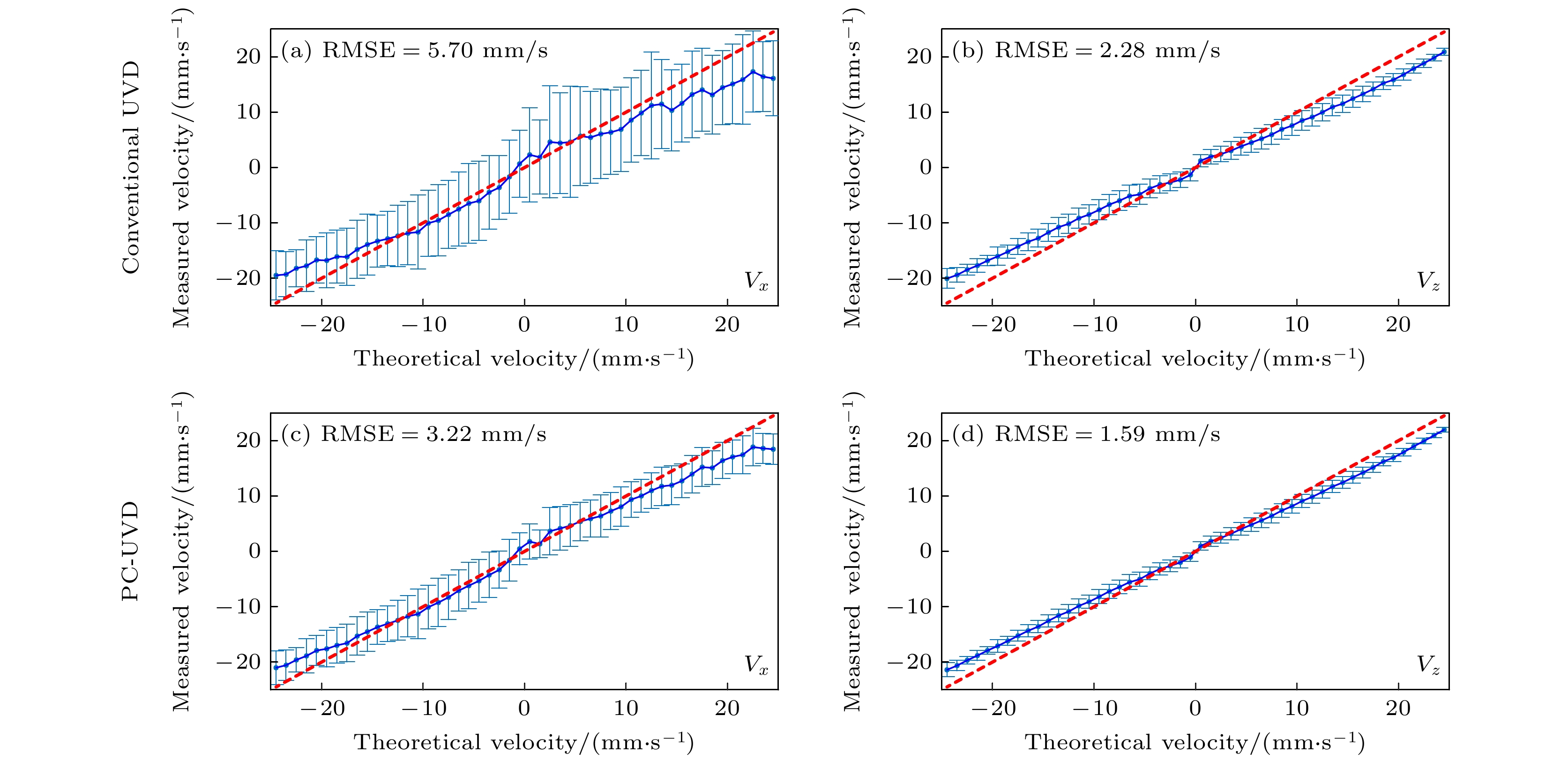
图 5 从螺旋流动模型中提取的速度矢量的精确度分析. 从螺旋血管内不同像素位置的速度值提取的(a), (c)水平分量和(b), (d)垂直分量与标准值的对比图; 误差条表示最少100次测量的标准偏差. 图中左上角展示了所有像素位置测量值的均方根误差. (a), (b)常规UVD测量结果分析; (c), (d) PC-UVD测量结果分析
Figure 5. Accuracy analysis of flow vectors derived from the spiral flow phantom. Plots of estimated velocity versus ground-truth velocity in (a), (c) lateral and (b), (d) axial directions, as extracted from the velocity values at different pixel positions within the spiral loop; error bars denote standard deviation over a minimum of 100 measurements. The RMSE of all pixel position measurements is demonstrated in the upper left corner of each of measurements at all pixel positions is displayed in the upper left corner of each plot: (a), (b) Analysis of results of conventional UVD; (c), (d) analysis of results of PC-UVD.
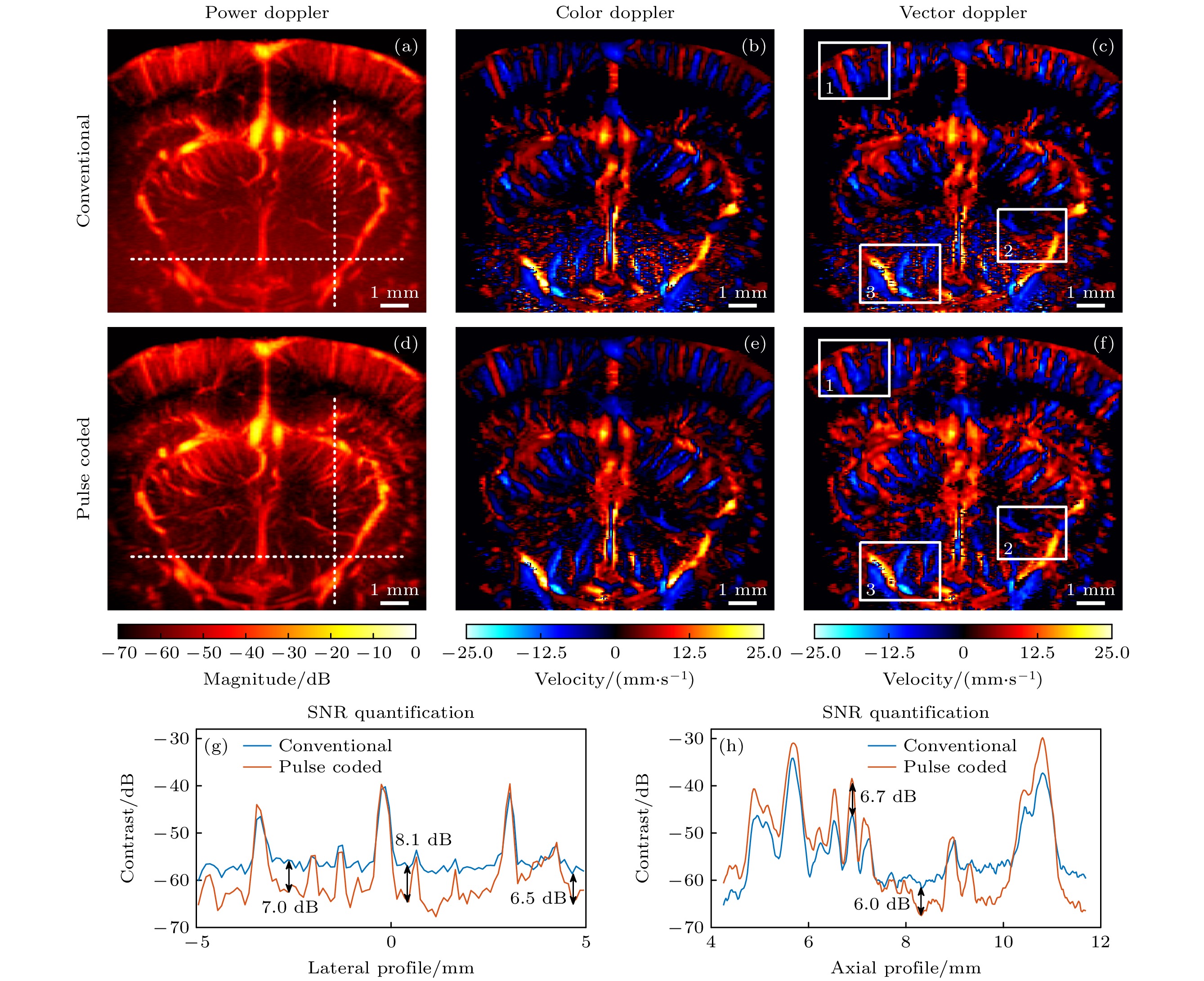
图 6 大鼠脑血流超快多普勒冠状切面成像结果 (a)—(c) 常规平面波发射模式下获得的超快(a)功率多普勒、(b)彩色多普勒和(c)矢量多普勒测量结果. (d)—(f) 多平面波脉冲编码发射模式下获得的超快(d)功率多普勒、(e)彩色多普勒和(f)矢量多普勒测量结果. 其中超快彩色多普勒和矢量多普勒测量结果图中红色和蓝色分别表示向上和向下的血流方向. (g) 图6(a)和图6(d)中水平虚线位置的信号强度剖面; (h) 图6(a)和图6(d)中竖直虚线位置的信号强度剖面
Figure 6. Ultrafast Doppler images of rat cerebral blood flow. (a)–(c) shows the ultrafast (a) power Doppler, (b) color Doppler, and (c) vector Doppler results obtained in conventional plane wave transmission mode. (d)–(f) presents the ultrafast (d) power Doppler, (e) color Doppler, and (f) vector Doppler results obtained in pulse coded plane wave transmission mode. In the ultrafast color Doppler and vector Doppler images, red and blue indicate upward and downward blood flow directions, respectively. (g) Signal intensity profile along the horizontal dashed line in Fig. 6(a) and Fig. 6(d); (h) signal intensity profile along the vertical dashed line in Fig. 6(a) and Fig. 6(d).
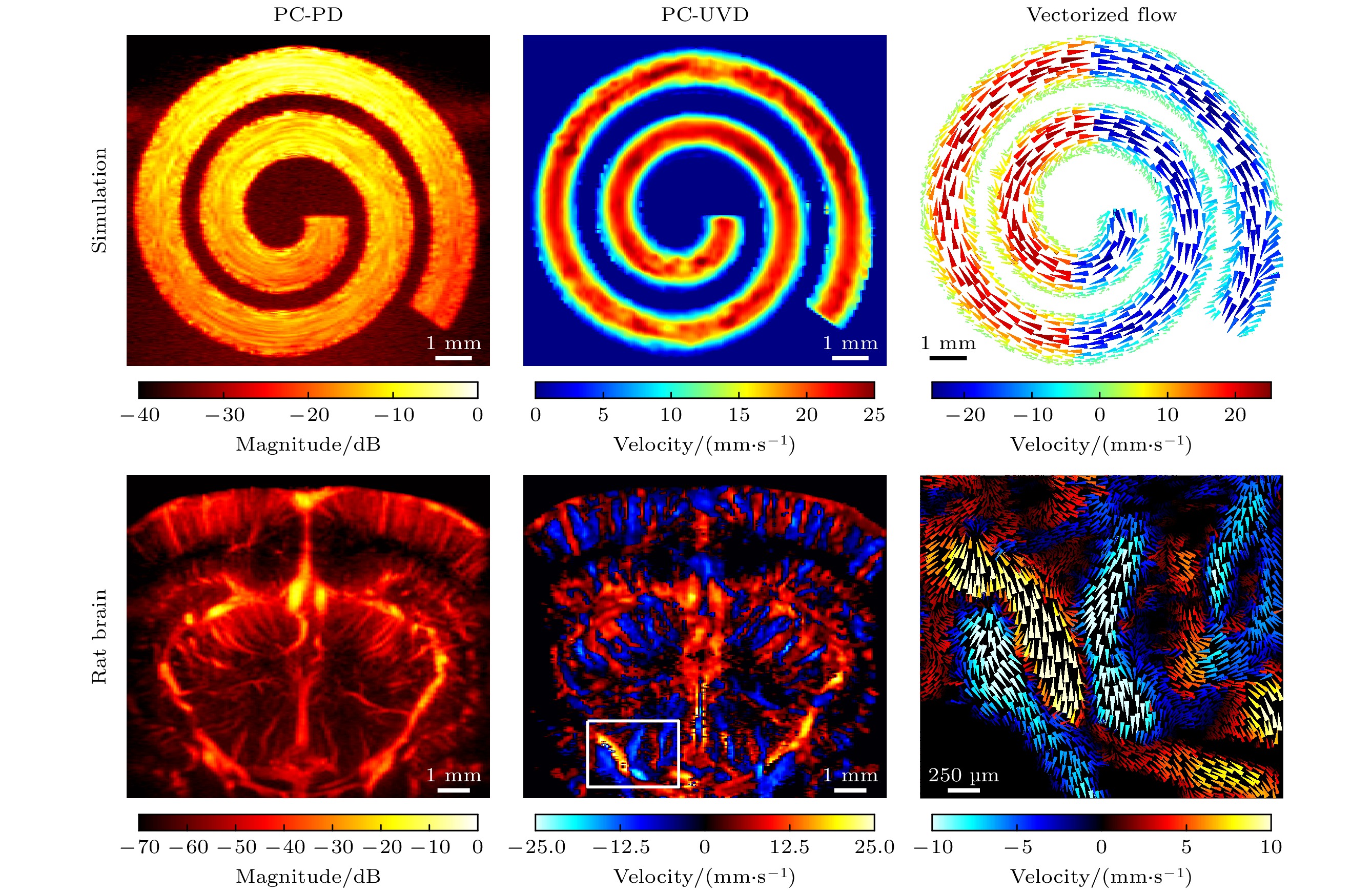
图 7 大鼠脑三个感兴趣区域(region of interest, ROI)的超快血流速度矢量化成像结果. 三个ROI分别对应了图6(c), (f)中三个矩形区域. (a)—(c)和(d)—(f)分别为基于常规UVD和PC-UVD方法获得的速度矢量测量结果. 用小三角形表示速度矢量, 三角形面积和颜色表示血流速度, 三角形锐角所指方向为血流速度方向
Figure 7. Ultrafast vectorized Doppler velocity imaging results in three ROIs in the rat brain. The three ROIs correspond to the three rectangular areas in Fig. 6(c) and Fig. 6(f). (a)–(c) shows the velocity measurements based on conventional UVD, while (d)–(f) shows the results based on PC-UVD. The velocity vectors are represented by small triangles, with the area and color indicating the magnitude of the blood flow velocity, and the sharp angles pointing in the direction of the flow.
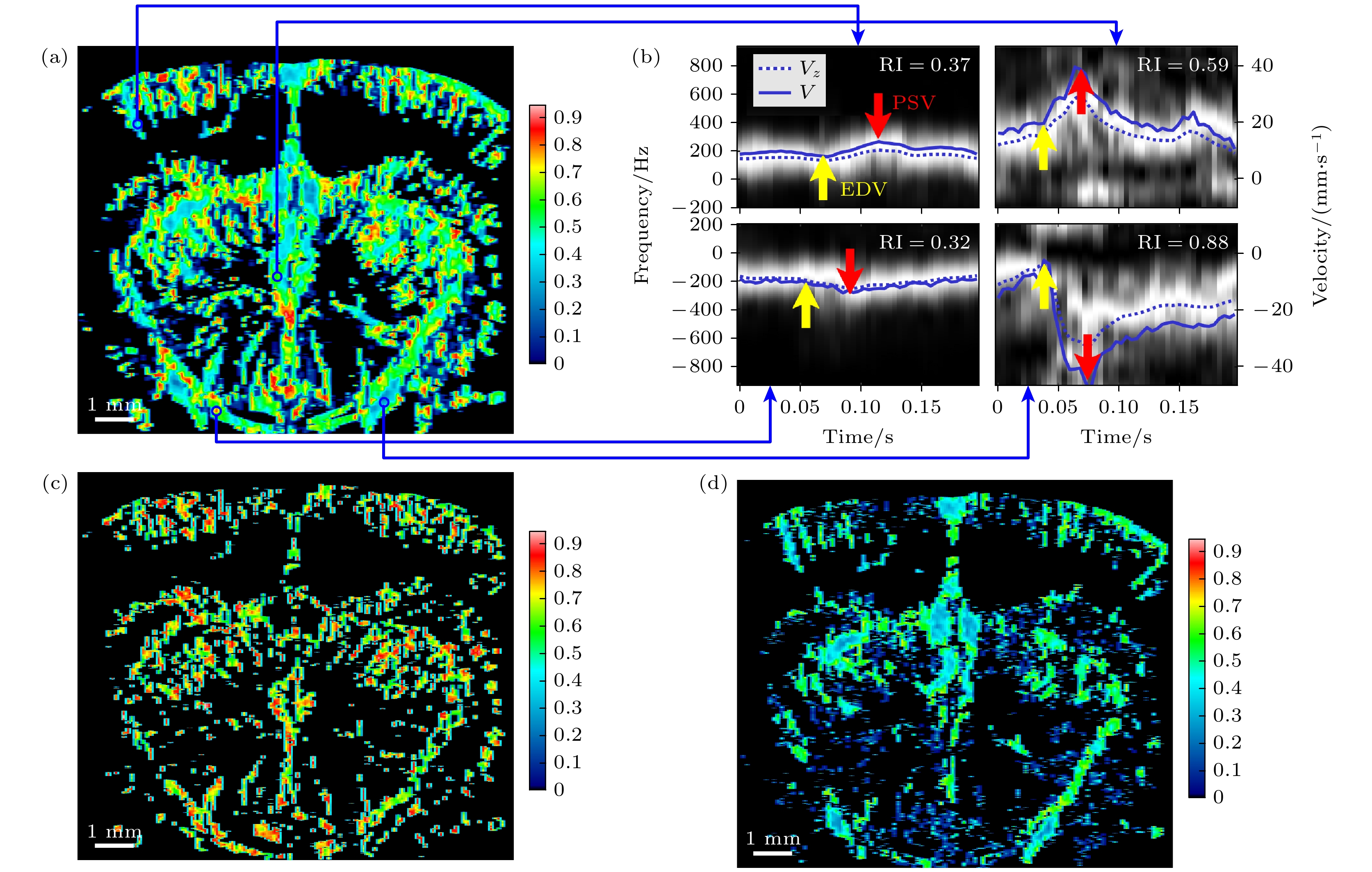
图 8 基于PC-UVD速度估计的大鼠脑血流阻抗指数测量结果 (a)血流阻抗指数图; (b)一个心动周期内, 不同位置的多角度相干复合后的血流多普勒频谱. 频谱中的虚线表示多普勒频谱的中心频率, 实线表示测量的矢量多普勒动态速度. 红色箭头指示心动周期内的血流峰值收缩速度, 黄色箭头指示血流舒张末期速度. 左上: 向上流的小静脉; 左下: 向下流的小静脉; 右上: 向上流的小动脉; 右下: 向下流的小动脉. (c)小动脉血流图. (d)小静脉血流图
Figure 8. Improved UVD based rat cerebral blood flow resistivity index measurements: (a) Cerebral blood flow resistivity index map; (b) multi-angle compounded Doppler spectra at different locations throughout a cardiac cycle. The dashed lines overlaid on the spectrum indicate the center frequency of the Doppler signal, while the solid lines represent the measured vector Doppler dynamic velocities. The red arrows point to the peak systolic blood flow velocity, and the yellow arrows point to the end-diastolic velocity. Top left: venous flow upward; bottom left: venous flow downward; top right: arterial flow upward; bottom right: arterial flow downward. (c) Arterial flow map. (d) Venous flow map.
表 1 仿真和大鼠实验参数设置
Table 1. Overview of parameters for simulation and rat experiments.
参数设置 仿真实验 大鼠实验 发射中心频率/MHz 15.625 15.625 脉冲重复频率/kHz 14.4 14.4 角度数 8 8 复合成像频率/kHz 1.8 1.8 采集时间/s 1/18 0.2 采集复合帧数 100 360 编码脉冲个数 8 8 脉冲间隔时间/μs 1 1 发射电压/V — 20 -
[1] Bandera E, Botteri M, Minelli C, Sutton A, Abrams K R, Latronico N 2006 Stroke 37 1334
 Google Scholar
Google Scholar
[2] Geurts L J, Zwanenburg J J M, Klijn C J M, Luijten P R, Biessels G J 2018 Stroke 50 1
 Google Scholar
Google Scholar
[3] Logothetis N K 2008 Nature 453 869
 Google Scholar
Google Scholar
[4] Salmela M B, Mortazavi S, Jagadeesan B D, Broderick D F, Burns J, Deshmukh T K, Harvey H B, Hoang J, Hunt C H, Kennedy T A, Khalessi A A, Mack W, Patel N D, Perlmutter J S, Policeni B, Schroeder J W, Setzen G, Whitehead M T, Cornelius R S, Corey A S 2017 J. Am. Coll. Radiol. 14 S34
 Google Scholar
Google Scholar
[5] Poelma C 2017 Exp. Fluids 58 1
 Google Scholar
Google Scholar
[6] Poelma C, van der Mijle R M E, Mari J M, Tang M X, Weinberg P D, Westerweel J 2012 Eur. J. Mech. B. Fluids 35 70
 Google Scholar
Google Scholar
[7] Omoto R, Kasai C 1986 Echocardiography 3 463
 Google Scholar
Google Scholar
[8] Kripfgans O D, Rubin J M, Hall A L, Fowlkes J B 2006 Ultrasound Med. Biol. 32 1037
 Google Scholar
Google Scholar
[9] Udesen J, Jensen J A 2006 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 53 959
 Google Scholar
Google Scholar
[10] Bohs L N, Geiman B J, Anderson M E, Gebhart S C, Trahey G E 2000 Ultrasonics 38 369
 Google Scholar
Google Scholar
[11] Fahrbach K 1969 Biomed. Tech. 14 233
 Google Scholar
Google Scholar
[12] Peronneau P, Bournat J, Bugnon A, Barbet A, Xhaard M 1974 Cardiovasc. Appl. Ultrasound 1 66
[13] Wang W Q, Yao L X 1982 Ultrasound Med. Biol. 8 421
 Google Scholar
Google Scholar
[14] Tsang I K H, Yiu B Y S, Yu A C H 2009 IEEE Int. Ultrason. Symp. 2009 1387
 Google Scholar
Google Scholar
[15] Bercoff J, Montaldo G, Loupas T, Savery D, Mézière F, Fink M, Tanter M 2011 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 58 134
 Google Scholar
Google Scholar
[16] Denarie B, Tangen T A, Ekroll I K, Rolim N, Torp H, Bjastad T, Lovstakken L 2013 IEEE Trans. Med. Imaging 32 1265
 Google Scholar
Google Scholar
[17] 臧佳琦, 许凯亮, 韩清见, 陆起涌, 梅永丰, 他得安 2021 70 114304
 Google Scholar
Google Scholar
Zang J Q, Xu K L, Han Q J, Lu Q Y, Mei Y F, Ta D A 2021 Acta Phys. Sin. 70 114304
 Google Scholar
Google Scholar
[18] Demene C, Deffieux T, Pernot M, Osmanski B F, Biran V, Gennisson J L, Sieu L A, Bergel A, Franqui S, Correas J M, Cohen I, Baud O, Tanter M 2015 IEEE Trans. Med. Imaging 34 2271
 Google Scholar
Google Scholar
[19] Sui Y H, Yan S Y, Yu J J, Song J P, Ta D A, Wang W Q, Xu K 2022 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 69 2425
 Google Scholar
Google Scholar
[20] Huang L J, Wang Y D, Wang R, Wei X Y, He Q, Zheng C C, Peng H, Luo J W 2023 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 70 378
 Google Scholar
Google Scholar
[21] Chen Y R, Fang B H, Meng F L, Luo J W, Luo X B 2024 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 71 459
 Google Scholar
Google Scholar
[22] 闫少渊, 许凯亮, 他得安 2023 复旦学报(自然科学版) 62 409
 Google Scholar
Google Scholar
Yan S Y, Xu K L, Ta D A 2023 J. Fudan Univ. (Nat. Sci.) 62 409
 Google Scholar
Google Scholar
[23] Yiu B Y, Yu A C 2016 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 63 1733
 Google Scholar
Google Scholar
[24] 王康宇, 周昱林, 何丽媛, 卢春尧, 于润, 吴大伟 2022 71 104303
 Google Scholar
Google Scholar
Wang K Y, Zhou Y L, He L Y, Lu C Y, Yu R, Wu D W 2022 Acta Phys. Sin. 71 104303
 Google Scholar
Google Scholar
[25] Yan S Y, Shou J J, Yu J J, Song J P, Mao Y, Xu K L 2023 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 70 613
 Google Scholar
Google Scholar
[26] Gong P, Song P F, Chen S G 2017 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 64 1674
 Google Scholar
Google Scholar
[27] Gong P, Song P F, Huang C W, Chen S G 2018 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 65 1977
 Google Scholar
Google Scholar
[28] Ferrara K, DeAngelis G 1997 Ultrasound Med. Biol. 23 321
 Google Scholar
Google Scholar
[29] Demene C, Pernot M, Biran V, Alison M, Fink M, Baud O, Tanter M 2014 J. Cereb. Blood Flow Metab. 34 1009
 Google Scholar
Google Scholar
[30] Jensen J A, Svendsen N B 1992 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 39 262
 Google Scholar
Google Scholar
[31] Jensen J A 1997 Med. Biol. Eng. Comput. 34 351
[32] Rabut C, Correia M, Finel V, Pezet S, Pernot M, Deffieux T, Tanter M 2019 Nat. Methods 16 994
 Google Scholar
Google Scholar
[33] Posada D, Poree J, Pellissier A, Chayer B, Tournoux F, Cloutier G, Garcia D 2016 IEEE Trans. Med. Imaging 35 1510
 Google Scholar
Google Scholar
[34] Poree J, Goudot G, Pedreira O, Laborie E, Khider L, Mirault T, Messas E, Julia P, Alsac J M, Tanter M, Pernot M 2021 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 68 2117
 Google Scholar
Google Scholar
[35] Ecarlat P, Perrot V, Carcreff E, Nicolas B, Liebgott H, Garcia D 2022 IEEE Int. Ultrason. Symp. 2022 1
 Google Scholar
Google Scholar
[36] Nahas H, Au J S, Ishii T, Yiu B Y S, Chee A J Y, Yu A C H 2020 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 67 2615
 Google Scholar
Google Scholar
[37] Nahas H, Ishii T, Yiu B Y S, Yu A C H 2023 IEEE Trans. Ultrason. Ferroelectr. Freq. Control 70 1384
 Google Scholar
Google Scholar
[38] 付亚鹏, 孙乾东, 李博艺, 他得安, 许凯亮 2023 72 074302
 Google Scholar
Google Scholar
Fu Y P, Sun Q D, Li B Y, Ta D A, Xu K L 2023 Acta Phys. Sin. 72 074302
 Google Scholar
Google Scholar
Catalog
Metrics
- Abstract views: 6123
- PDF Downloads: 128
- Cited By: 0













 DownLoad:
DownLoad: