-
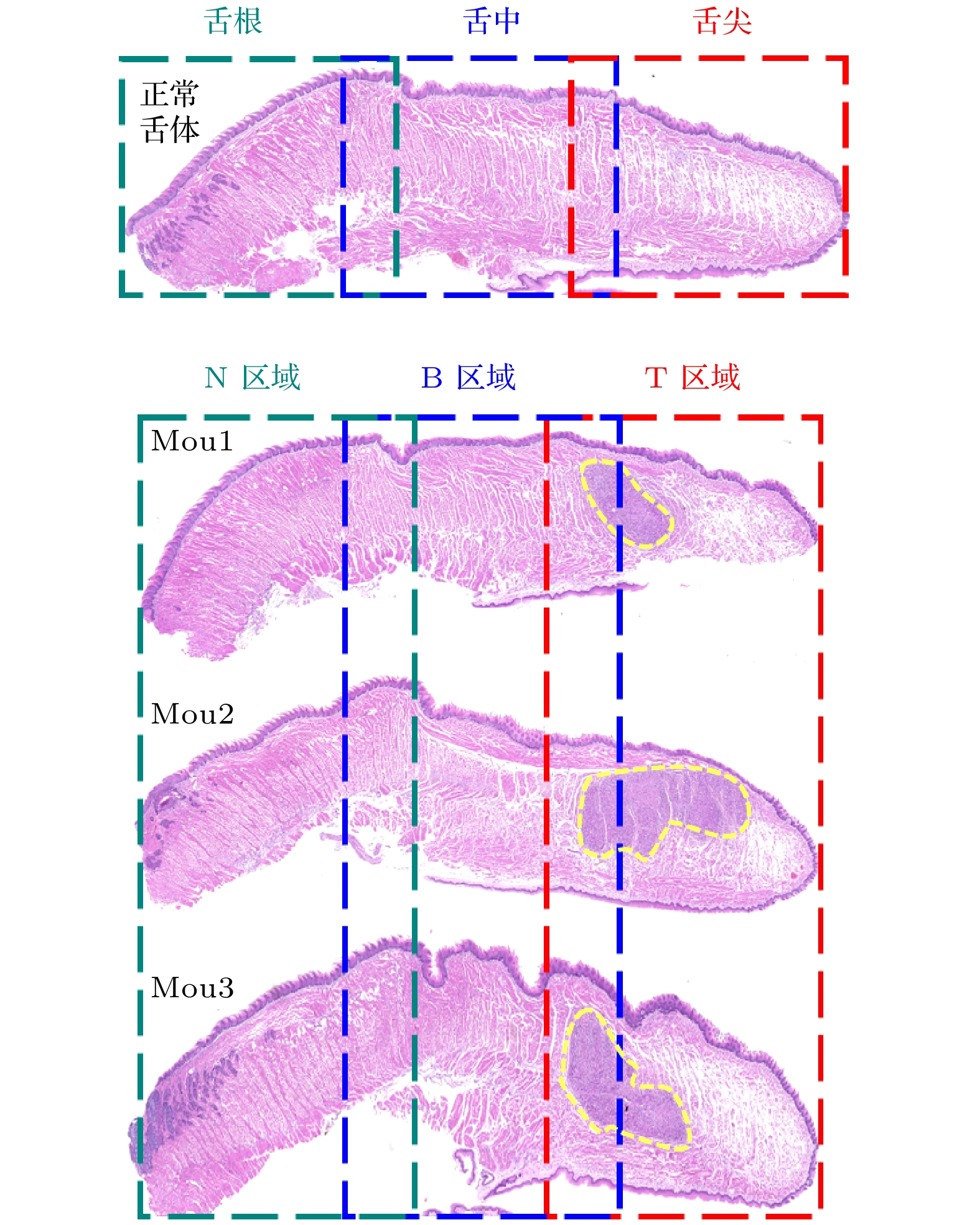
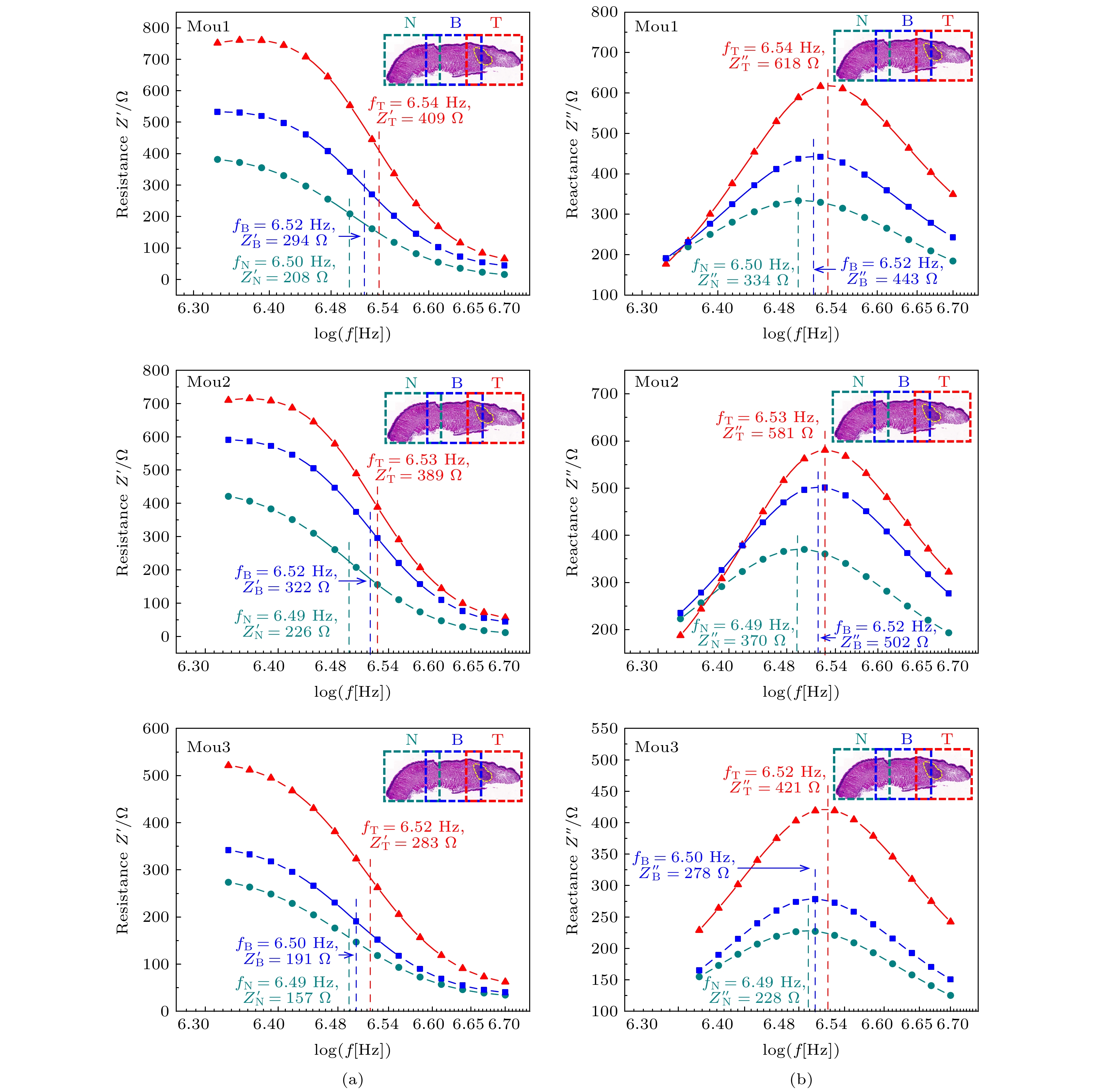
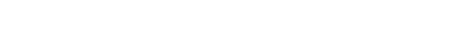
基于生物阻抗谱技术, 提出一种非侵入式、快速、便捷的舌体肿瘤组织识别方法. 根据舌体组织不同病理及生理状态下电学特性的差异性来判断其是否病变, 以帮助主刀医师在临床舌体肿瘤手术切除中既能完整的切除肿瘤又能尽可能多的保留患者舌功能. 本文在小鼠上建立了人舌鳞癌细胞(HSC3)原位舌癌移植瘤模型, 用生物阻抗谱的方法对其正常组织区域、混有肿瘤组织区域及肿瘤组织区域进行了电学特性研究. 幅值频谱显示在8.09 × 105 —5 × 106 Hz的高频段可以根据其电学特性区分3种组织. 在实验过程中, 从高频段的幅值频谱中提取出弛豫频率frelax、电阻抗实部
${{{Z}}'_{\rm{relax}}}$ 和电阻抗虚部${{{Z}}''_{\rm{relax}}}$ 3个电学参数, 并根据这3个电学参数定义癌变组织系数α与β (待测组织阻抗值相对于正常组织阻抗值的实部变化百分比记为α, 虚部相对变化百分比记为β)进行肿瘤组织识别. 结果表明, 当α ≤ 36.5%, β ≤ 31.2%时, 组织是正常组织; 当α ≥ 36.5%, β ≥ 31.2%时, 组织可能混有肿瘤组织; 当α ≥ 82.7%, β ≥ 73.6%时, 组织是肿瘤组织.A fast and convenient method of recognizing the tongue tumor tissue based on bioelectrical impedance spectroscopy (BIS) is proposed. According to the difference among the electrical characteristics of tongue tissue under different pathological and physiological conditions, we can judge whether it is pathological. This method can help the surgeon in the clinical resection of tongue cancer not only to remove the tumor completely, but also to retain the patient’s tongue function as much as possible. In this paper, a model of human tongue squamous cell carcinoma (HSC3) xenografted in situ is established in mice. The electrical properties of the normal tissue, mixed tumor tissue and tumor tissue are studied by the BIS technology. The amplitude spectrum shows that none of the three tissues can be distinguished well in a low frequency range of 100–8.09 × 105 Hz due to the influence of contact impedance, but they can be distinguished according to their electrical characteristics in a high frequency range of 8.09 × 105–5 × 106 Hz. In the process of the experiment, first of all, the tip, middle and root of the normal tongue are detected, and the results show that the impedance values of these three parts are similar in the high frequency band, so the influence of different positions of tongue on the impedance value can be excluded. Then, the same three regions of the cancerous tongue are detected, and three electrical parameters, namely relaxation frequency frelax, real part spectrum${{{Z}}'_{\rm{relax}}}$ and imaginary part spectrum${{{Z}}''_{\rm{relax}}}$ of electrical impedance are extracted from the amplitude spectrum of high frequency band. The quantitative analyses of these three kinds of tissues show that the${{{Z}}'_{\rm{relax}}}$ and${{{Z}}''_{\rm{relax}}}$ of tumor tissue are the highest, and those of normal tissue are the lowest. Finally, the cancerous tissue coefficients α and β (the relative change percentage of the real part and imaginary part of the impedance value between the tested tissue and normal tissue) are determined according to these three electrical parameters for tumor tissue identification. The results show that when α ≤ 36.5% and β ≤ 31.2%, the tissue is normal; when α ≥ 36.5% and β ≥ 31.2%, the tissue may be mixed with tumor tissue; when α ≥ 82.7% and β ≥ 73.6%, the tissue is tumor tissue.-
Keywords:
- tongue cancer /
- bioelectrical impedance spectroscopy /
- electrical properties /
- relaxation frequency
[1] Koyama S, Tabuchi T, Okawa S, Morishima T, Ishimoto S, Ishibashi M, Miyashiro I 2020 Oral Oncol. 105 104653
 Google Scholar
Google Scholar
[2] 贾琼, 顾晓明 2011 辽宁医学院学报 32 280
 Google Scholar
Google Scholar
Jia Q, Gu X M 2011 J. Liaoning Med. Coll. 32 280
 Google Scholar
Google Scholar
[3] Samołyk-Kogaczewska N, Sierko E, Zuzda K, et al. 2019 Strahlenther. Onkol. 195 780
 Google Scholar
Google Scholar
[4] Shibuya Y, Tanimoto H, Umeda M, Yokoo S, Komori T 2004 Kobe J. Med. Sci. 50 1
[5] Noorlag R, Nulent T J W K, Delwel V E J, Pameijer F A, Es R J J V 2020 Oral Oncol. 110 104895
 Google Scholar
Google Scholar
[6] Yesuratnam A, Wiesenfeld D, Tsui A, Iseli T A, Hoorn S V, Ang M T, Guiney A, Phal P M 2014 Int. J. Oral Surg. 43 787
 Google Scholar
Google Scholar
[7] Mao M H, Wang S, Feng Z E, Li J Z, Li H, Qin L Z, Han Z X 2019 Oral Oncol. 91 79
 Google Scholar
Google Scholar
[8] Murakami R, Shiraishi S, Yoshida R, Sakata J, Yamana K, Hirosue A, Uchiyama Y, Nakayama H, Yamashita Y 2019 Acad. Radiol. 26 e180
 Google Scholar
Google Scholar
[9] Tarabichi O, Bulbul M G, Kanumuri V V, et al. 2019 Laryngoscope 129 662
 Google Scholar
Google Scholar
[10] Locatello L G, Bruno C, Pietragalla M, et al. 2020 Oral Oncol. 107 104749
 Google Scholar
Google Scholar
[11] Fu J Y, Zhu L, Li J, et al. 2020 Br. J. Oral Maxillofac. Surg. 58 997
 Google Scholar
Google Scholar
[12] Furusawa J, Oridate N, SuZuki F, Homma A, Furuta Y, Fukuda S 2007 Oral Oncol. 44 793
[13] Baba A, Ojiri H, Ogane S, Hashimoto K, Inoue T, Takagiwa M, Goto T K 2021 Oral Radiol. 37 86
 Google Scholar
Google Scholar
[14] Wang L, Hu S, Liu K, Chen B, Wu H, Jia J, Yao J 2020 Rev. Sci. Instrum. 91 124104
 Google Scholar
Google Scholar
[15] 姚佳烽, 万建芬, 杨璐, 刘凯, 陈柏, 吴洪涛 2020 69 163301
 Google Scholar
Google Scholar
Yao J F, Wan J F, Yang L, Liu K, Chen B, Wu H T 2020 Acta Phys. Sin. 69 163301
 Google Scholar
Google Scholar
[16] Mahdavi R, Hosseinpour P, Abbasvandi F, MehrvarZ S, Abdolahad M J 2020 Biosens. Bioelectron. 165 112421
 Google Scholar
Google Scholar
[17] 陈玉娟, 王晓东, 吴剑, 付峰, 朱彩蓉, 蒲洋, 向飞, 戴涛 2016 四川大学学报 47 267
Chen Y J, Wang X D, Wu J, Fu F, Zhu C R, Pu Y, Xiang F, Dai T 2016 J. Sichuan.Univ. 47 267
[18] 李翔, 刘锋, 帅建伟 2016 65 178704
 Google Scholar
Google Scholar
Li X, Liu F, Shuai J W 2016 Acta Phys. Sin. 65 178704
 Google Scholar
Google Scholar
[19] Wang Y, Zhang W, Sun P, Cai Y, Xu W, Fan Q, Hu Q, Han W 2019 Theranostics 9 391
 Google Scholar
Google Scholar
[20] Liu X, Yao J, Zhao T, Obara H, Cui Y, Takei M 2018 IEEE Trans. Biomed. Circuits Syst. 12 623
 Google Scholar
Google Scholar
-
图 5 HSC3癌变舌体组织电学特性对比 (a)弛豫频率 frelax对比; (b)电阻抗实部
$ {Z'_{\rm{relax}}} $ 对比; (c)电阻抗虚部$ {Z''_{\rm{relax}}} $ 对比Fig. 5. Comparison of the electrical characteristics of tongue tissue in HSC3 canceration: (a) Comparison of frelax; (b) comparison of
$ {Z'_{\rm{relax}}} $ ; (c) comparison of$ {Z''_{\rm{relax}}} $ 表 1 阻抗测量值的最大相对误差
Table 1. Maximum relative error of impedance value.
组织区域 最大相对误差/% Mou1 Mou2 Mou3 N区域 2.65 4.45 2.68 B区域 2.54 1.36 2.77 T区域 1.24 1.73 3.95 -
[1] Koyama S, Tabuchi T, Okawa S, Morishima T, Ishimoto S, Ishibashi M, Miyashiro I 2020 Oral Oncol. 105 104653
 Google Scholar
Google Scholar
[2] 贾琼, 顾晓明 2011 辽宁医学院学报 32 280
 Google Scholar
Google Scholar
Jia Q, Gu X M 2011 J. Liaoning Med. Coll. 32 280
 Google Scholar
Google Scholar
[3] Samołyk-Kogaczewska N, Sierko E, Zuzda K, et al. 2019 Strahlenther. Onkol. 195 780
 Google Scholar
Google Scholar
[4] Shibuya Y, Tanimoto H, Umeda M, Yokoo S, Komori T 2004 Kobe J. Med. Sci. 50 1
[5] Noorlag R, Nulent T J W K, Delwel V E J, Pameijer F A, Es R J J V 2020 Oral Oncol. 110 104895
 Google Scholar
Google Scholar
[6] Yesuratnam A, Wiesenfeld D, Tsui A, Iseli T A, Hoorn S V, Ang M T, Guiney A, Phal P M 2014 Int. J. Oral Surg. 43 787
 Google Scholar
Google Scholar
[7] Mao M H, Wang S, Feng Z E, Li J Z, Li H, Qin L Z, Han Z X 2019 Oral Oncol. 91 79
 Google Scholar
Google Scholar
[8] Murakami R, Shiraishi S, Yoshida R, Sakata J, Yamana K, Hirosue A, Uchiyama Y, Nakayama H, Yamashita Y 2019 Acad. Radiol. 26 e180
 Google Scholar
Google Scholar
[9] Tarabichi O, Bulbul M G, Kanumuri V V, et al. 2019 Laryngoscope 129 662
 Google Scholar
Google Scholar
[10] Locatello L G, Bruno C, Pietragalla M, et al. 2020 Oral Oncol. 107 104749
 Google Scholar
Google Scholar
[11] Fu J Y, Zhu L, Li J, et al. 2020 Br. J. Oral Maxillofac. Surg. 58 997
 Google Scholar
Google Scholar
[12] Furusawa J, Oridate N, SuZuki F, Homma A, Furuta Y, Fukuda S 2007 Oral Oncol. 44 793
[13] Baba A, Ojiri H, Ogane S, Hashimoto K, Inoue T, Takagiwa M, Goto T K 2021 Oral Radiol. 37 86
 Google Scholar
Google Scholar
[14] Wang L, Hu S, Liu K, Chen B, Wu H, Jia J, Yao J 2020 Rev. Sci. Instrum. 91 124104
 Google Scholar
Google Scholar
[15] 姚佳烽, 万建芬, 杨璐, 刘凯, 陈柏, 吴洪涛 2020 69 163301
 Google Scholar
Google Scholar
Yao J F, Wan J F, Yang L, Liu K, Chen B, Wu H T 2020 Acta Phys. Sin. 69 163301
 Google Scholar
Google Scholar
[16] Mahdavi R, Hosseinpour P, Abbasvandi F, MehrvarZ S, Abdolahad M J 2020 Biosens. Bioelectron. 165 112421
 Google Scholar
Google Scholar
[17] 陈玉娟, 王晓东, 吴剑, 付峰, 朱彩蓉, 蒲洋, 向飞, 戴涛 2016 四川大学学报 47 267
Chen Y J, Wang X D, Wu J, Fu F, Zhu C R, Pu Y, Xiang F, Dai T 2016 J. Sichuan.Univ. 47 267
[18] 李翔, 刘锋, 帅建伟 2016 65 178704
 Google Scholar
Google Scholar
Li X, Liu F, Shuai J W 2016 Acta Phys. Sin. 65 178704
 Google Scholar
Google Scholar
[19] Wang Y, Zhang W, Sun P, Cai Y, Xu W, Fan Q, Hu Q, Han W 2019 Theranostics 9 391
 Google Scholar
Google Scholar
[20] Liu X, Yao J, Zhao T, Obara H, Cui Y, Takei M 2018 IEEE Trans. Biomed. Circuits Syst. 12 623
 Google Scholar
Google Scholar
计量
- 文章访问数: 8387
- PDF下载量: 122
- 被引次数: 0
















 下载:
下载: