-
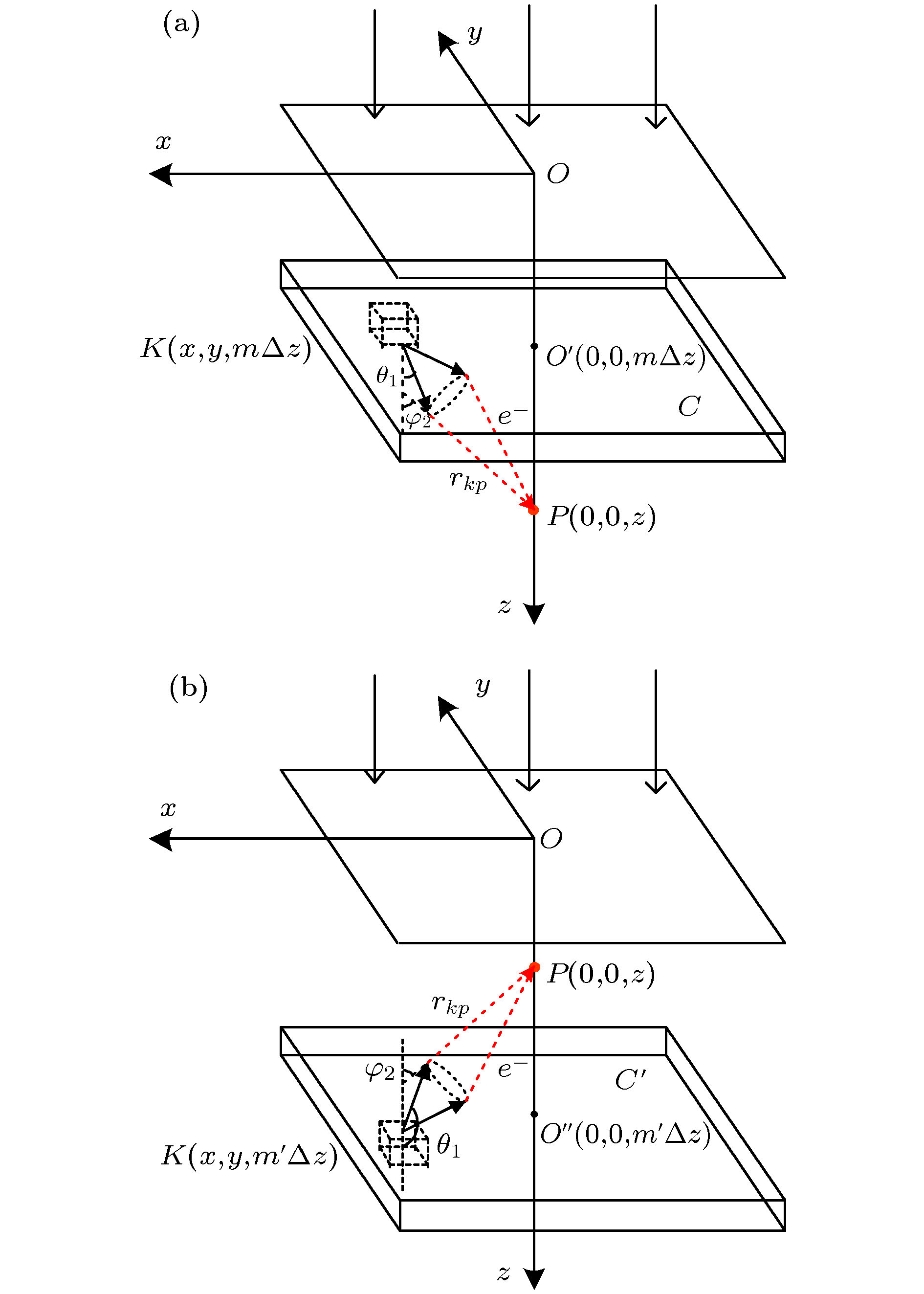
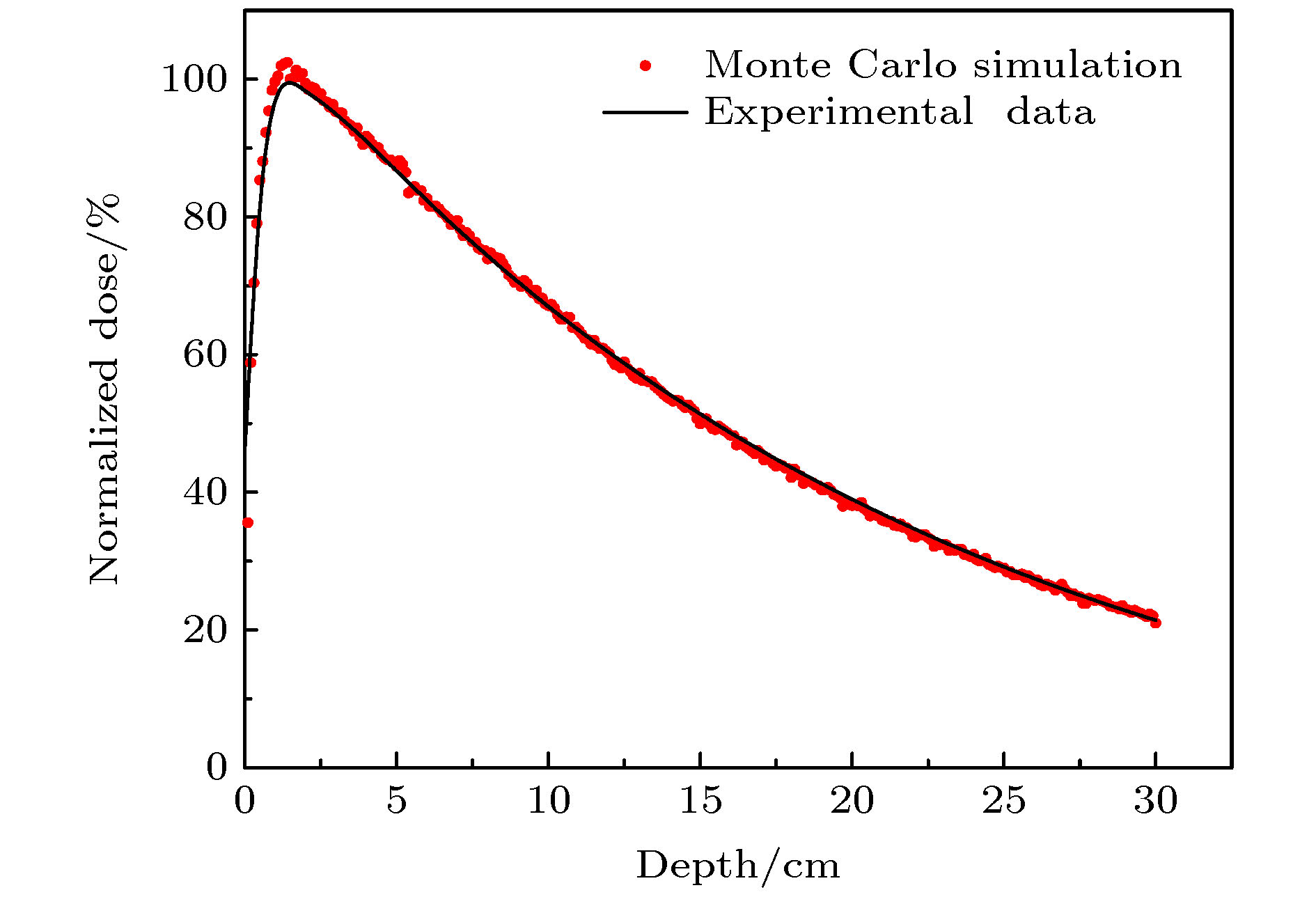
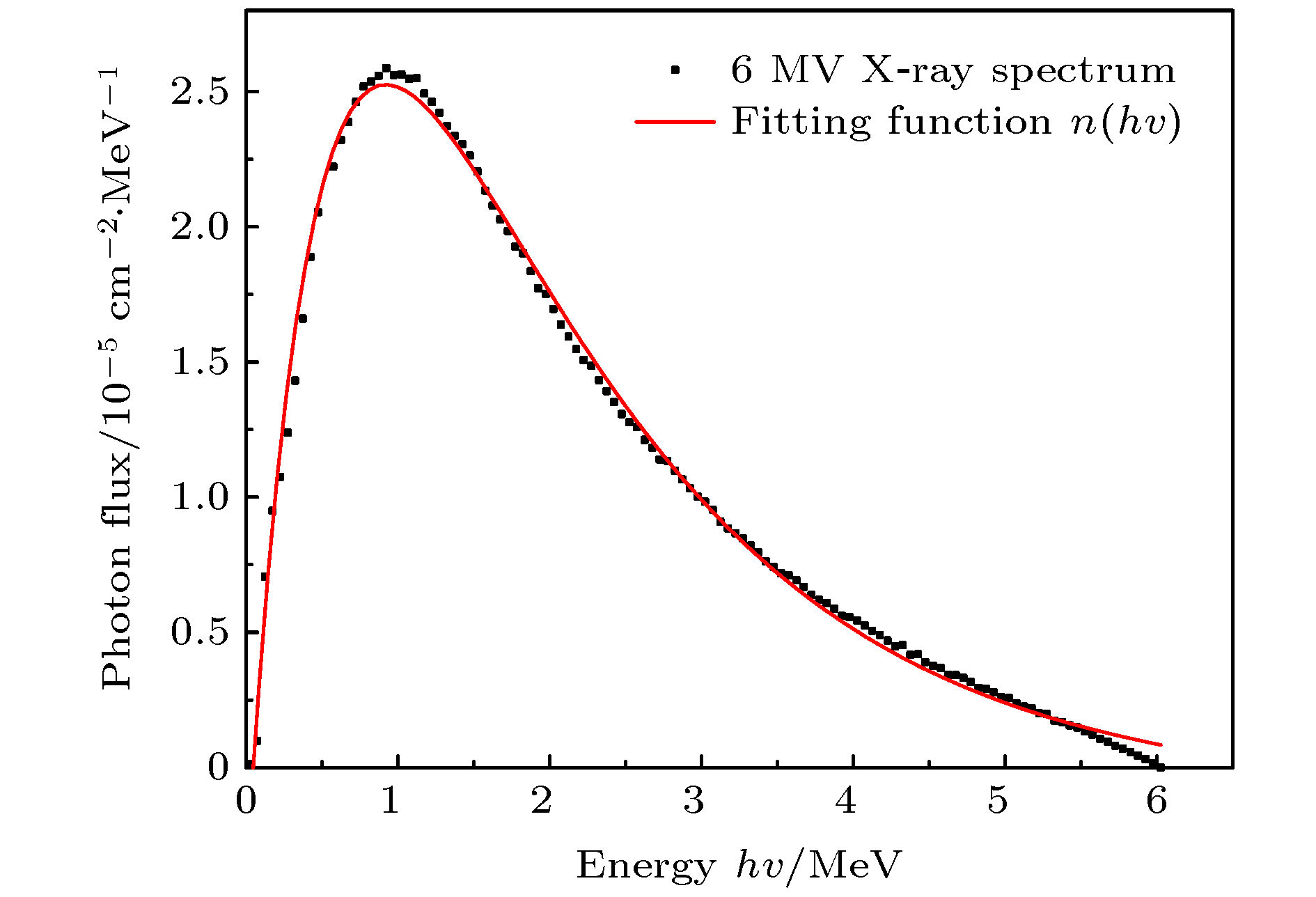
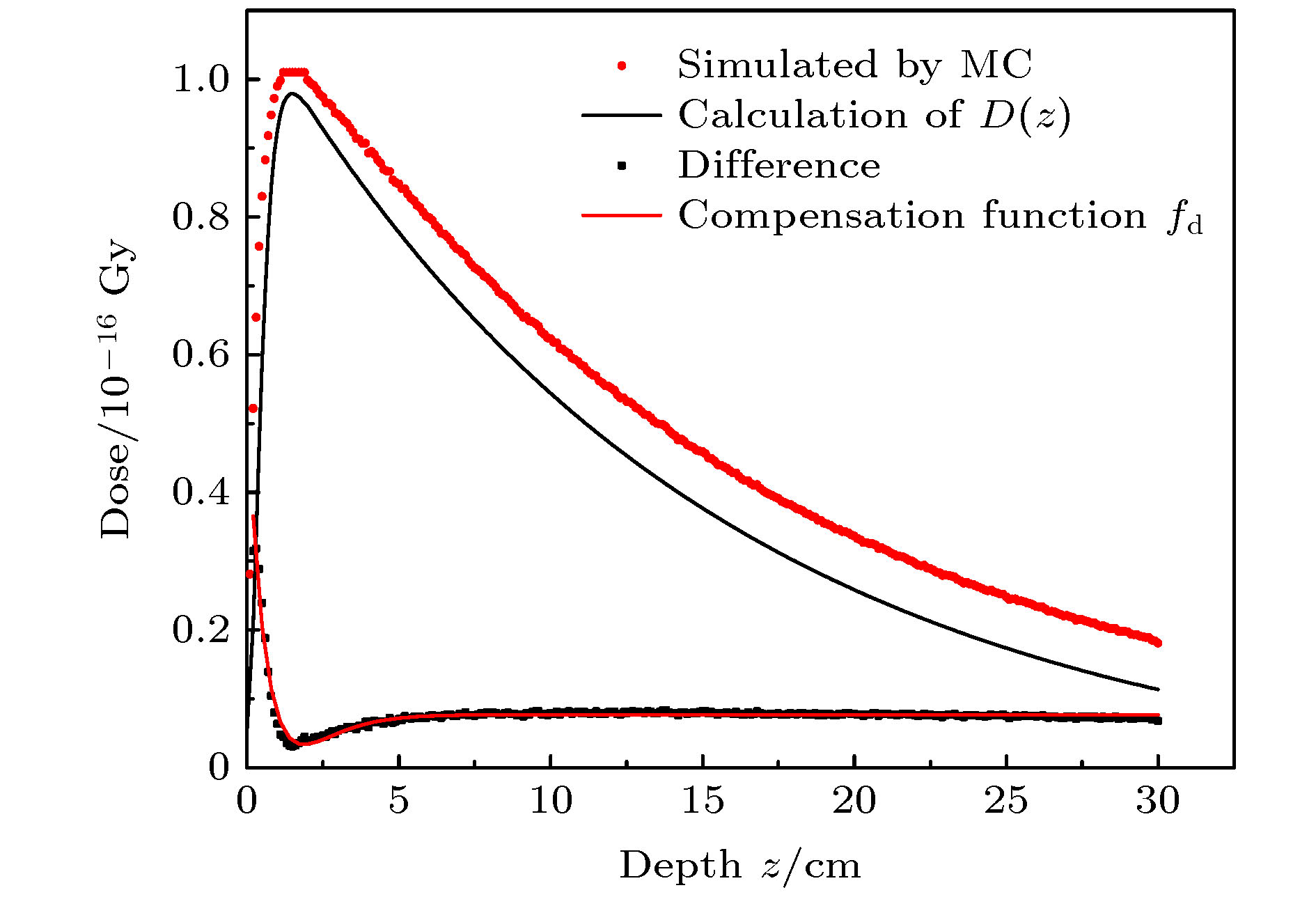
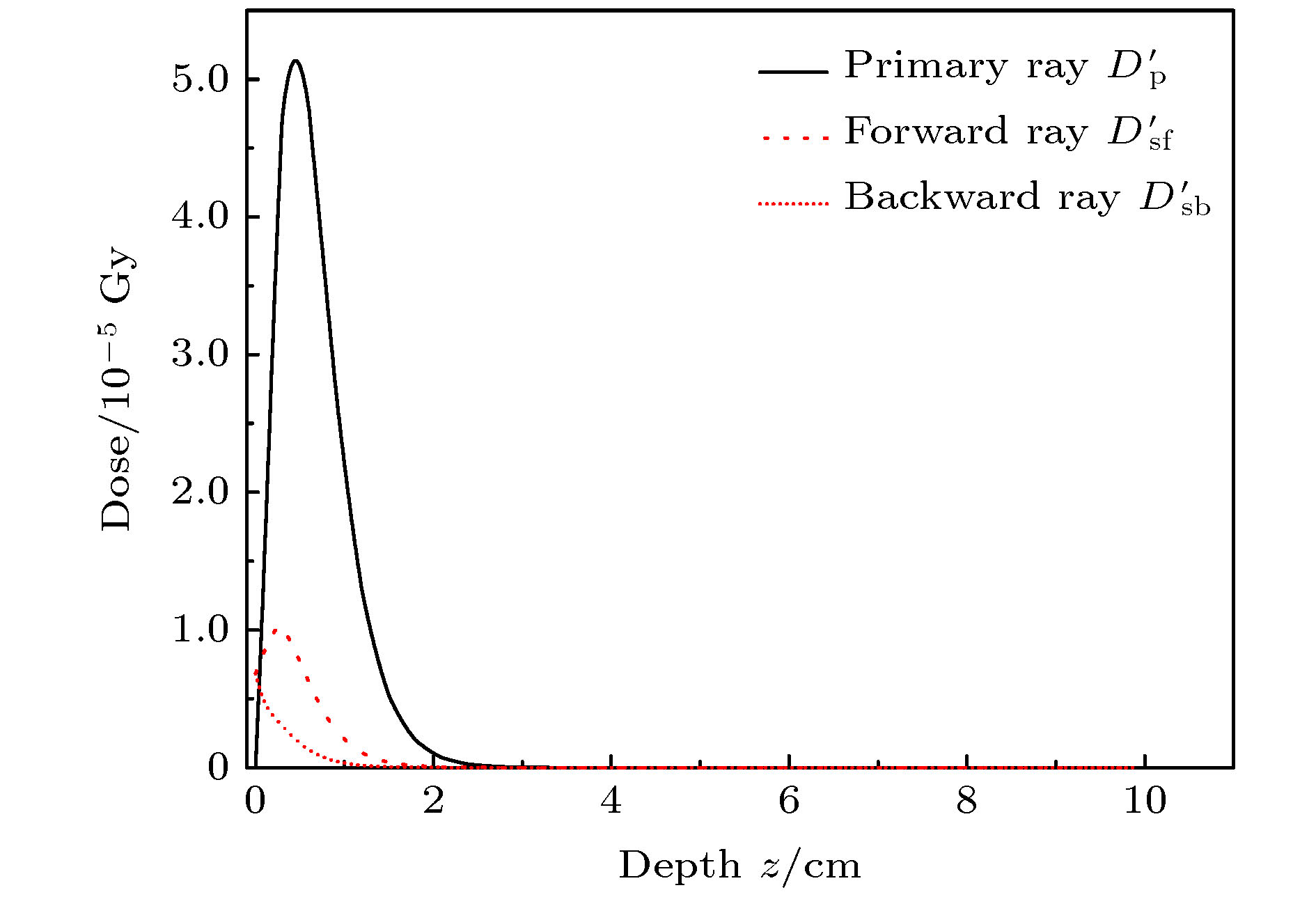
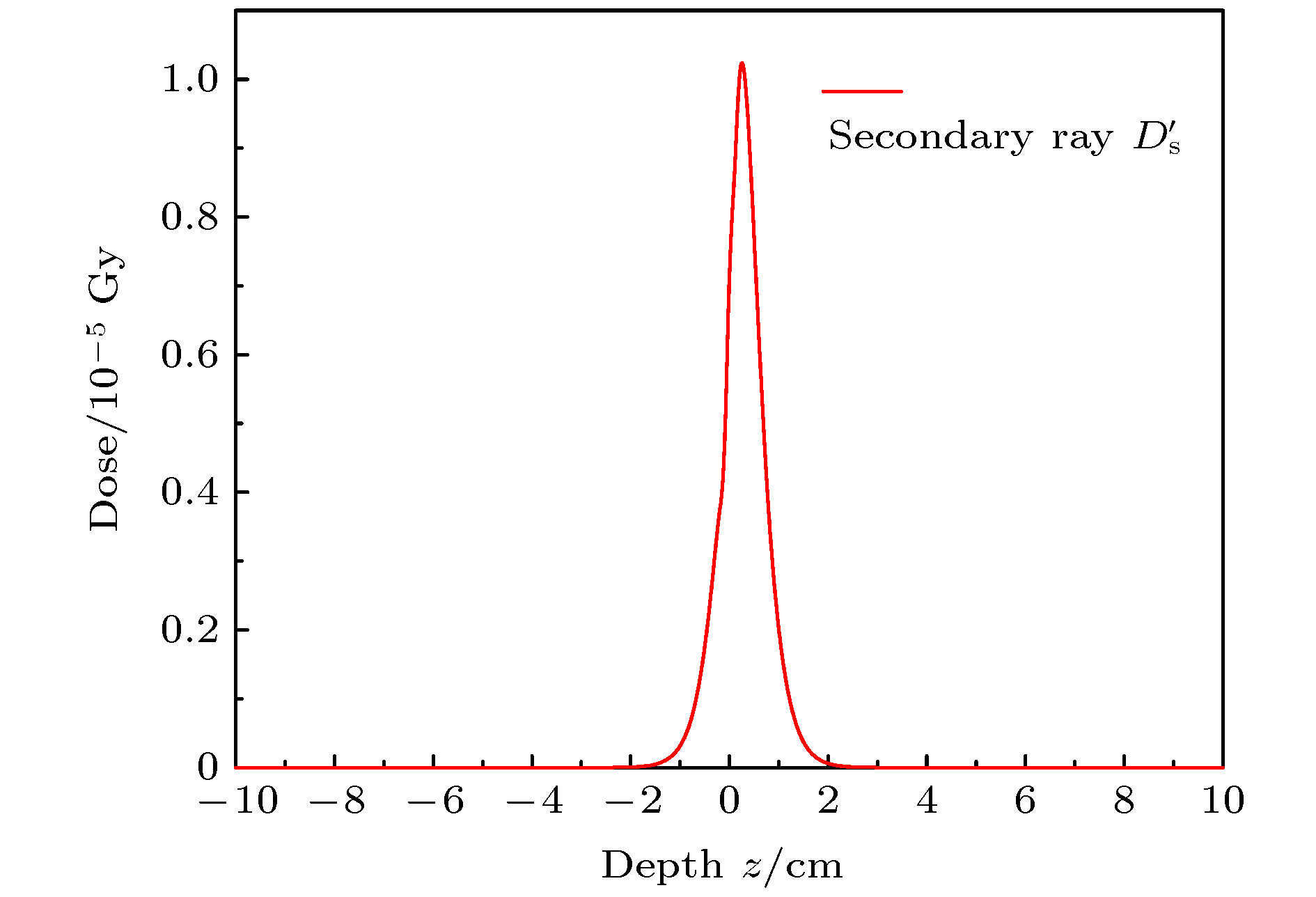
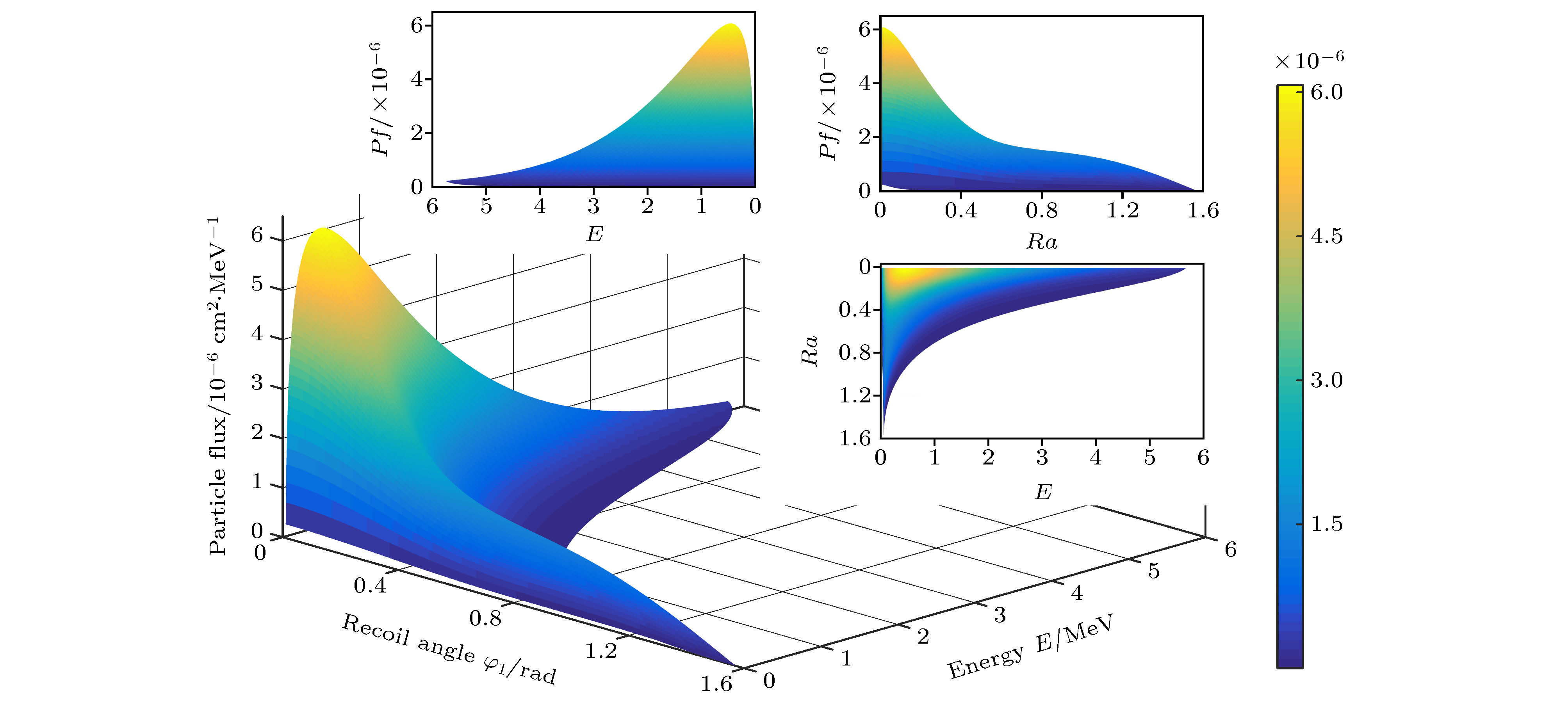
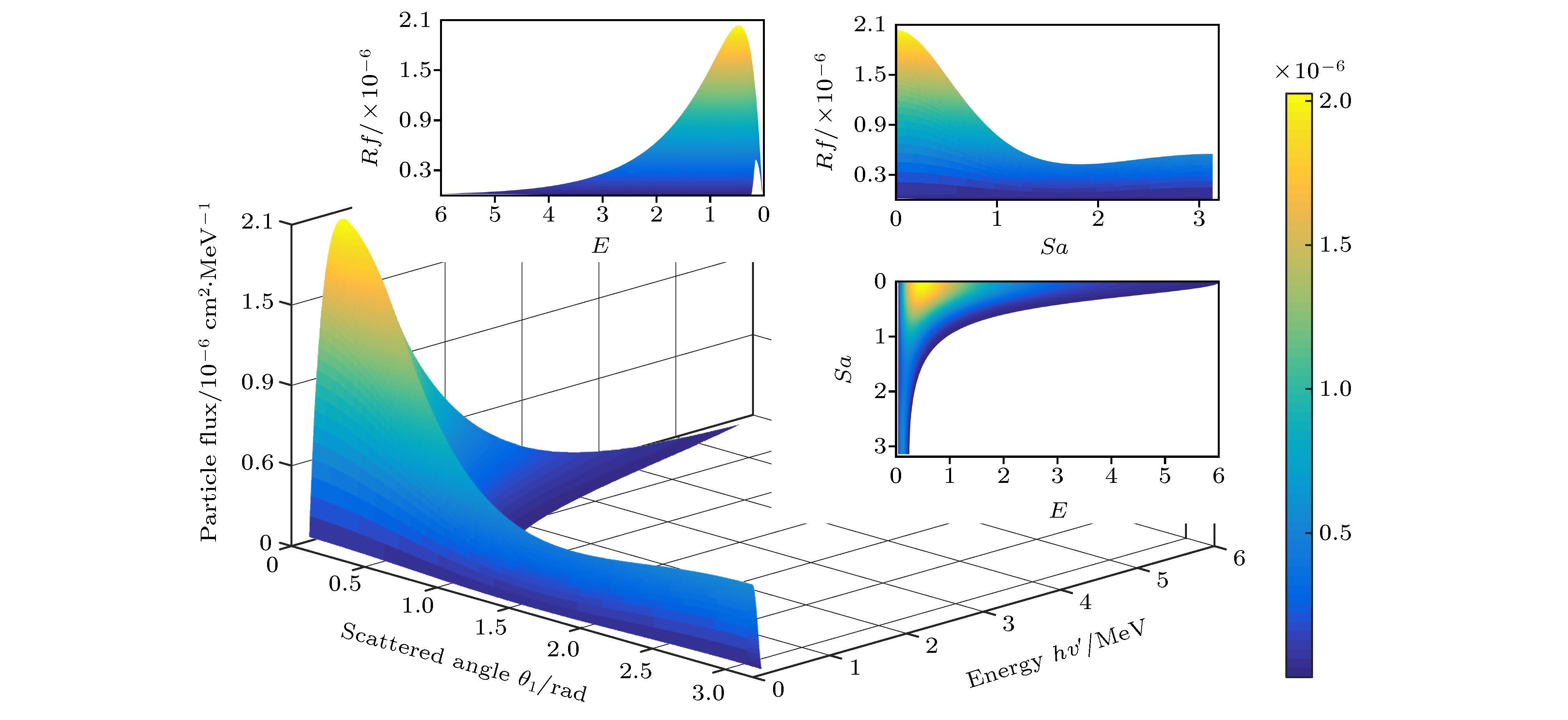
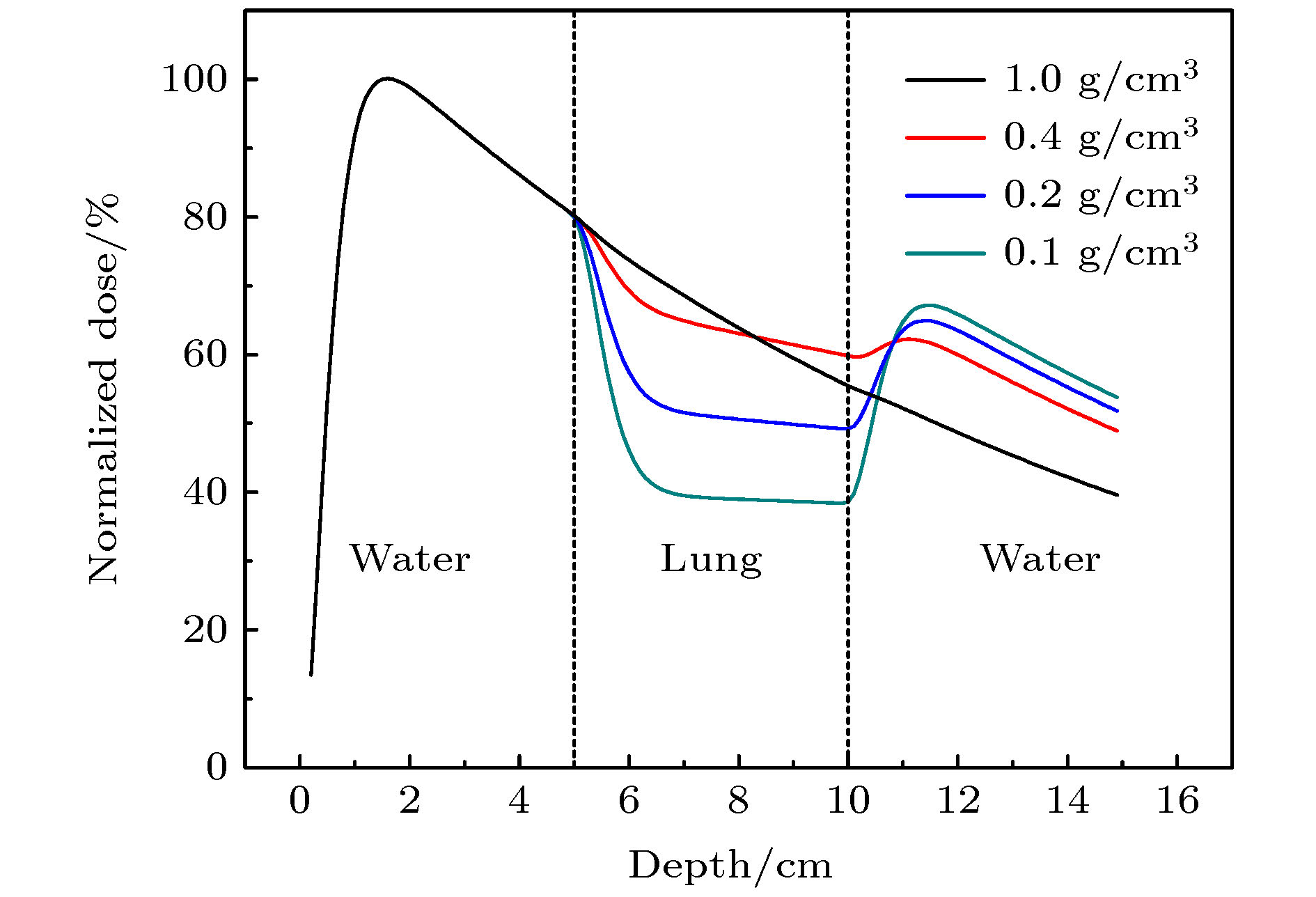
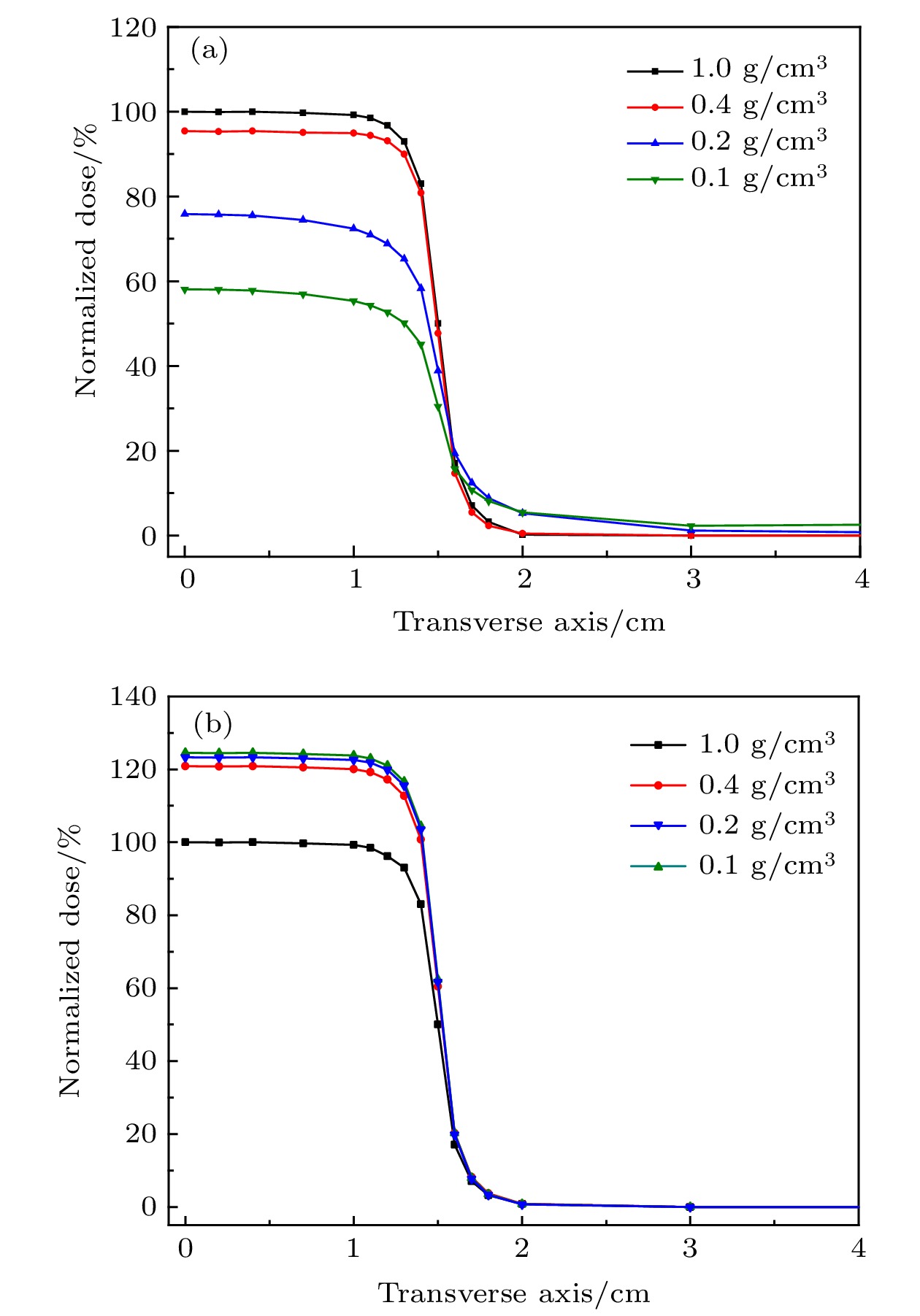
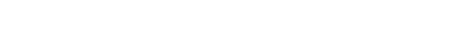
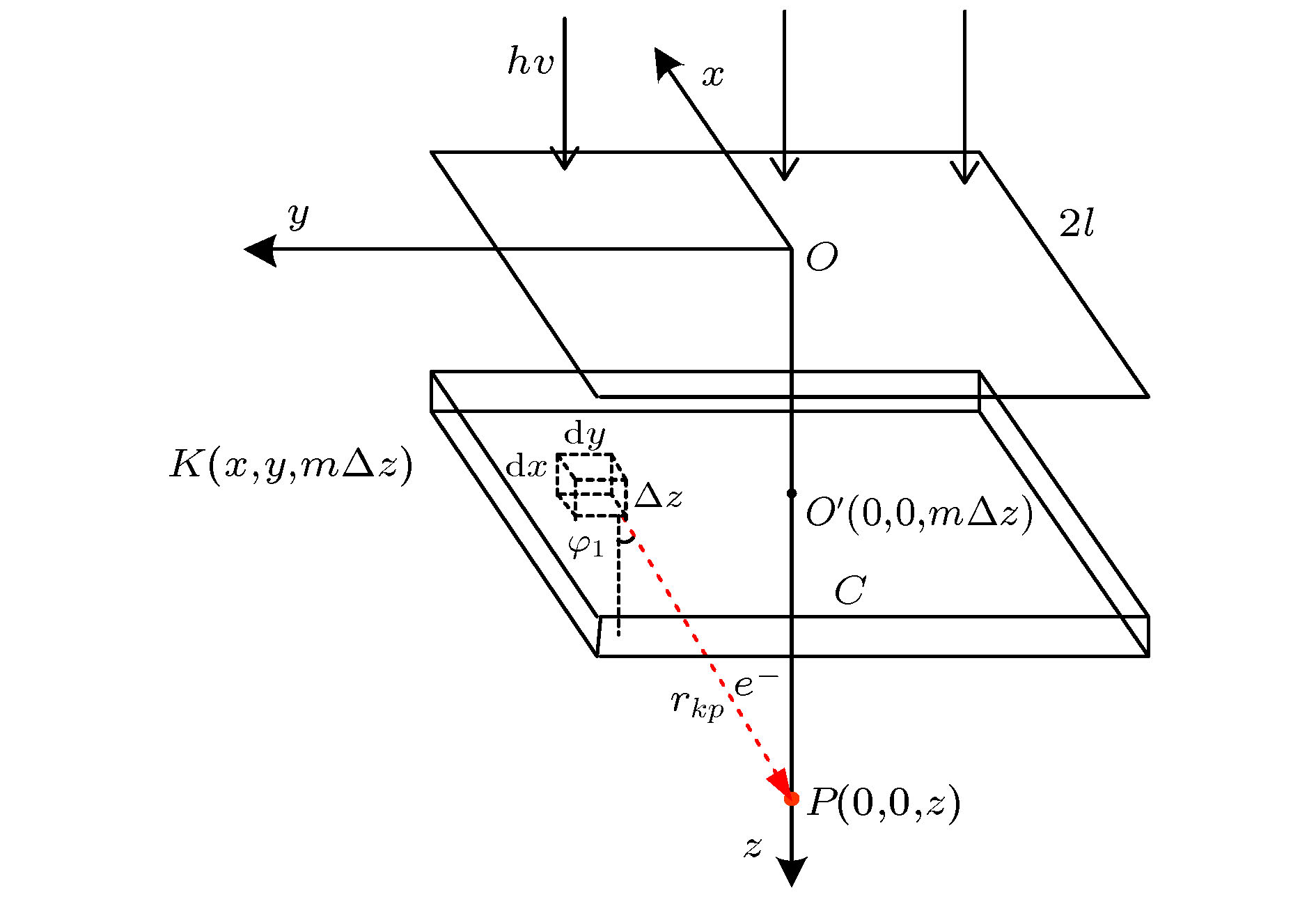
本文提出一种通过物理模型计算放疗过程中每一个组织深度处绝对剂量的算法, 它可代替蒙特卡罗仿真的部分工作且耗费时间更少. 这个算法是基于对照射野内X射线产生电子的能量注量的积分运算, 并考虑了射线的能谱及二次散射线, 得到了后向散射对表面剂量的贡献比例, 同时得到前向散射、后向散射及原射线剂量贡献的关系. 比较了二次光子和二次电子的三维能谱, 得出该能谱是粒子注量关于粒子能量和粒子运动方向的函数. 为了得到每一深度处的光子注量, 计算了有连续能谱的X射线的期望质量衰减系数. 上述算法计算得到的绝对剂量与蒙特卡罗方式仿真的结果趋势一致, 两者的差异在于算法未考虑高于二次的散射线. 最后将算法应用到非均匀模体剂量计算, 能准确反映其中剂量分布特点且具有较小的误差.A algorithm of obtaining absolute dose at each tissue depth only by the mathematical calculation of formula is reported. The algorithm is based on integrating the energy flux of the electron generated by X-ray in the range of irradiation field, and the energy spectrum of ray and the secondary scattered ray are considered in this process. In this algorithm, the water phantom in the irradiation field is divided into several thin layers, and the energy flux of the electrons generated by interaction between the ray and thin layer reaching the calculation point is calculated. Finally, the absolute dose of the calculation point can be obtained by accumulating the energy flux contribution of all thin layers. For the X-ray with continuous energy spectrum, the expected mass attenuation coefficient is calculated for obtaining the photon flux at each depth in this process. The absolute dose calculated by this algorithm is verified by Monte Carlo simulation, and the difference between the algorithm and simulation is compensated for by a dose function about multiple scattering photons, and the function shows fast descent and then slow ascent. It is found that the ratio of the dose caused by backscatter to the surface dose, and the relationship among forward scatter, backward scatter and primary ray, and the relationship between the dose and the depth of the secondary scattered rays show a trend of first rising and then declining, and the depth of the peak value deviates from the position of the thin layer. Three-dimensional energy spectra of the secondary photon and the secondary electron are also compared with each other, and the spectrum is a function of particle flux about particle energy and particle direction. From the perspective of Compton effect, the physical meanings of different positions in the three-dimensional energy spectrum of the two particles are explained. It is found that the difference between algorithm percentage depth dose and simulation percentage depth dose is similar to the difference between small irradiation field percentage depth dose and big irradiation field percentage depth dose from simulation, and it is verified that the difference between algorithm and simulation comes from the increase of scattered rays. Finally, the algorithm is applied to the dose calculation of non-uniform phantom, which can accurately reflect the dose distribution characteristics and have less error.
-
Keywords:
- radiotherapy /
- model /
- absolute dose /
- Compton effect
[1] Yamamoto T, Mizowaki T, Miyabe Y, Takegawa H, Narita Y, Yano S, Nagata Y, Teshima T, Hiraoka M 2007 Phys. Med. Biol. 52 1991
 Google Scholar
Google Scholar
[2] Einstein A J, Henzlova M J, Rajagopalan S 2007 JAMA 298 317
 Google Scholar
Google Scholar
[3] Delaney G, Jacob S, Featherstone C, Barton M 2005 Cancers 104 1129
 Google Scholar
Google Scholar
[4] Das I J, Cheng C W, Watts R J, Ahnesjo A, Gibbons J, Li X A, Lowenstein J, Mitra R K, Simon W E, Zhu T C 2008 Med. Phys. 35 4186
 Google Scholar
Google Scholar
[5] van't Veld A A, van Luijk P, Praamstra F, van der Hulst P C 2001 Med. Phys. 28 738
 Google Scholar
Google Scholar
[6] van't Veld A A, van Luijk P, Praamstra F, van der Hulst P C 2000 Med. Phys. 27 923
 Google Scholar
Google Scholar
[7] Jette D 2000 Med. Phys. 27 1705
 Google Scholar
Google Scholar
[8] Jette D 1999 Med. Phys. 26 924
 Google Scholar
Google Scholar
[9] Tillikainen L, Helminen H, Torsti T, Siljamaki S, Alakuijala J, Pyyry J, Ulmer W 2008 Phys. Med. Biol. 53 3821
 Google Scholar
Google Scholar
[10] Jones A O, Das I J 2005 Med. Phys. 32 766
 Google Scholar
Google Scholar
[11] Aarup L R, Nahum A E, Zacharatou C, Juhler-Nottrup T, Knoos T, Nystrom H, Specht L, Wieslander E, Korreman S S 2009 Radiother. Oncol. 91 405
 Google Scholar
Google Scholar
[12] Krieger T, Sauer O A 2005 Phys. Med. Biol. 50 859
 Google Scholar
Google Scholar
[13] Beilla S, Younes T, Vieillevigne L, Bardies M, Franceries X, Simon L 2017 Phys. Medica 41 46
 Google Scholar
Google Scholar
[14] Jansen A A 1980 Icru Report 33: Radiation Quantities and Units (Washington)
[15] 胡逸民 1999 肿瘤放射物理学 (北京: 原子能出版社) 第38−44页
Hu Y M 1999 Radiation Oncology Physics (Beijing: Atomic Energy Press) pp38−44(in Chinese)
[16] Attix F H 1986 Gamma- and X-Ray Interactions in Matter (Vol.1) (Weinheim: Wiley-VCH Verlag GmbH & Co.KgaA) pp125−38
[17] Price M J, Hogstrom K R, Antolak J A, White R A, Bloch C D, Boyd R A 2007 J. Appl. Clin. Med. Phys 8 61
 Google Scholar
Google Scholar
[18] Malataras G, Kappas C, Lovelock D M J 2001 Phys. Med. Biol. 46 2435
 Google Scholar
Google Scholar
[19] Cheng C W, Cho S H, Taylor M, Das I J 2007 Med. Phys. 34 3149
 Google Scholar
Google Scholar
[20] Carlone M, Tadic T, Keller H, Rezaee M, Jaffray D 2016 Med. Phys. 43 2927
 Google Scholar
Google Scholar
[21] Kinhikar R A 2008 Technol. Cancer Res. Treat. 7 381
 Google Scholar
Google Scholar
[22] Chow J C L, Grigorov G N, Barnett R B 2006 Med. Dosim. 31 249
 Google Scholar
Google Scholar
[23] Disher B, Hajdok G, Gaede S, Battista J J 2012 Phys. Med. Biol. 57 1543
 Google Scholar
Google Scholar
[24] Mesbahi A, Dadgar H, Ghareh-Aghaji N, Mohammadzadeh M 2014 J. Cancer Res. Ther. 10 896
 Google Scholar
Google Scholar
-
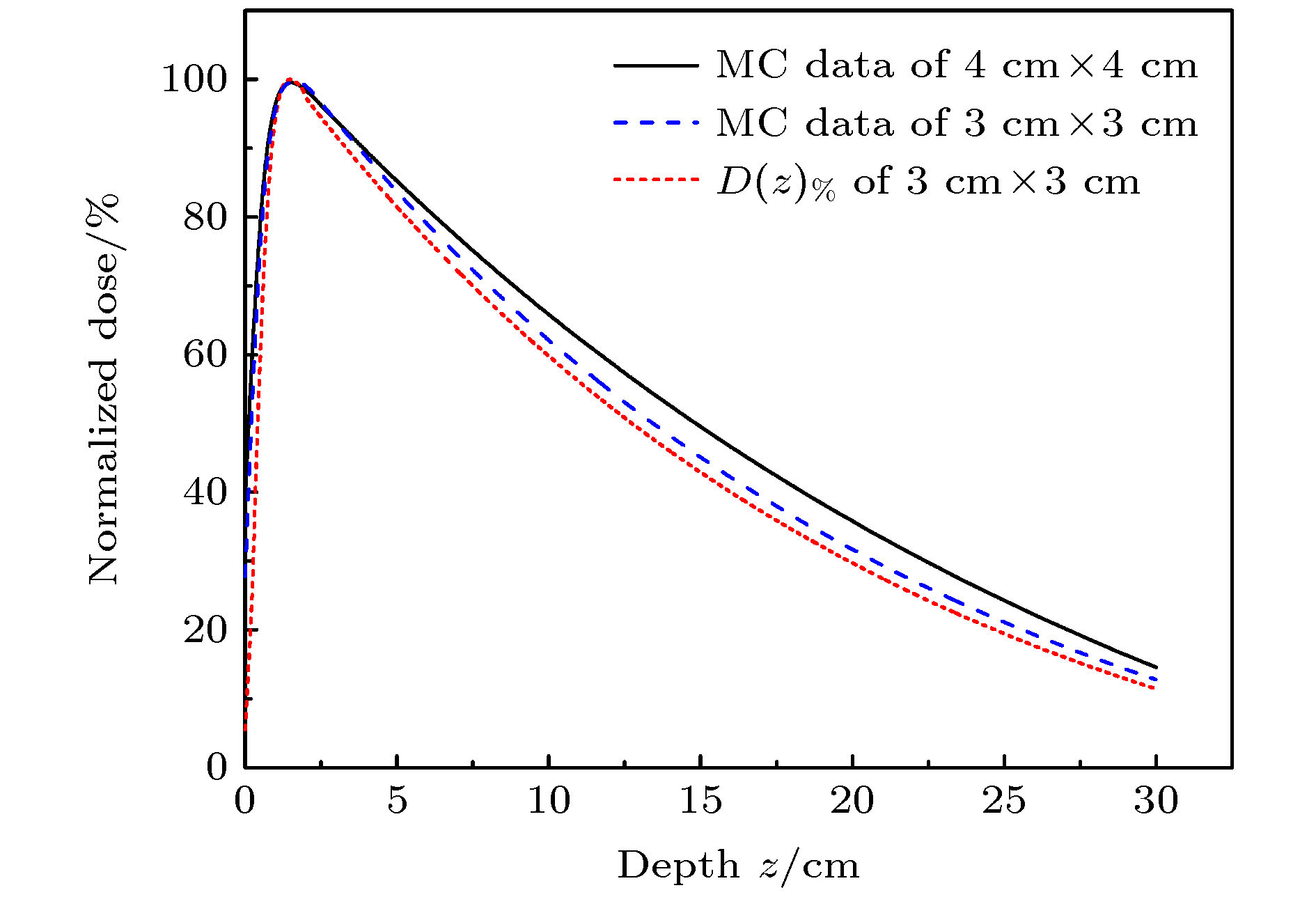
图 10 比较随不同射野(射野大小3 cm × 3 cm和4 cm × 4 cm)变化的蒙特卡罗仿真数据
$ {D}_{\mathrm{M}\mathrm{C}} $ 与计算的$ D{\left(z\right)}_{\%} $ (射野大小3 cm × 3 cm)Fig. 10. Comparison of Monte Carlo simulation PDD with different fields (field size 3 cm × 3 cm and 4 cm × 4 cm) and calculation PDD
$ D{\left(z\right)}_{\%} $ (field size 3 cm × 3 cm).表 1 不同肺模体密度ρ对应参数kρ和μ0
Table 1. Parameters kρ and μ0 of lung phantom densities ρ.
ρ/g·cm–3 0.1 0.2 0.4 ≥ ρT kρ –6 –3.75 0.75 3 μ0 6.8 6.1 4.7 4 -
[1] Yamamoto T, Mizowaki T, Miyabe Y, Takegawa H, Narita Y, Yano S, Nagata Y, Teshima T, Hiraoka M 2007 Phys. Med. Biol. 52 1991
 Google Scholar
Google Scholar
[2] Einstein A J, Henzlova M J, Rajagopalan S 2007 JAMA 298 317
 Google Scholar
Google Scholar
[3] Delaney G, Jacob S, Featherstone C, Barton M 2005 Cancers 104 1129
 Google Scholar
Google Scholar
[4] Das I J, Cheng C W, Watts R J, Ahnesjo A, Gibbons J, Li X A, Lowenstein J, Mitra R K, Simon W E, Zhu T C 2008 Med. Phys. 35 4186
 Google Scholar
Google Scholar
[5] van't Veld A A, van Luijk P, Praamstra F, van der Hulst P C 2001 Med. Phys. 28 738
 Google Scholar
Google Scholar
[6] van't Veld A A, van Luijk P, Praamstra F, van der Hulst P C 2000 Med. Phys. 27 923
 Google Scholar
Google Scholar
[7] Jette D 2000 Med. Phys. 27 1705
 Google Scholar
Google Scholar
[8] Jette D 1999 Med. Phys. 26 924
 Google Scholar
Google Scholar
[9] Tillikainen L, Helminen H, Torsti T, Siljamaki S, Alakuijala J, Pyyry J, Ulmer W 2008 Phys. Med. Biol. 53 3821
 Google Scholar
Google Scholar
[10] Jones A O, Das I J 2005 Med. Phys. 32 766
 Google Scholar
Google Scholar
[11] Aarup L R, Nahum A E, Zacharatou C, Juhler-Nottrup T, Knoos T, Nystrom H, Specht L, Wieslander E, Korreman S S 2009 Radiother. Oncol. 91 405
 Google Scholar
Google Scholar
[12] Krieger T, Sauer O A 2005 Phys. Med. Biol. 50 859
 Google Scholar
Google Scholar
[13] Beilla S, Younes T, Vieillevigne L, Bardies M, Franceries X, Simon L 2017 Phys. Medica 41 46
 Google Scholar
Google Scholar
[14] Jansen A A 1980 Icru Report 33: Radiation Quantities and Units (Washington)
[15] 胡逸民 1999 肿瘤放射物理学 (北京: 原子能出版社) 第38−44页
Hu Y M 1999 Radiation Oncology Physics (Beijing: Atomic Energy Press) pp38−44(in Chinese)
[16] Attix F H 1986 Gamma- and X-Ray Interactions in Matter (Vol.1) (Weinheim: Wiley-VCH Verlag GmbH & Co.KgaA) pp125−38
[17] Price M J, Hogstrom K R, Antolak J A, White R A, Bloch C D, Boyd R A 2007 J. Appl. Clin. Med. Phys 8 61
 Google Scholar
Google Scholar
[18] Malataras G, Kappas C, Lovelock D M J 2001 Phys. Med. Biol. 46 2435
 Google Scholar
Google Scholar
[19] Cheng C W, Cho S H, Taylor M, Das I J 2007 Med. Phys. 34 3149
 Google Scholar
Google Scholar
[20] Carlone M, Tadic T, Keller H, Rezaee M, Jaffray D 2016 Med. Phys. 43 2927
 Google Scholar
Google Scholar
[21] Kinhikar R A 2008 Technol. Cancer Res. Treat. 7 381
 Google Scholar
Google Scholar
[22] Chow J C L, Grigorov G N, Barnett R B 2006 Med. Dosim. 31 249
 Google Scholar
Google Scholar
[23] Disher B, Hajdok G, Gaede S, Battista J J 2012 Phys. Med. Biol. 57 1543
 Google Scholar
Google Scholar
[24] Mesbahi A, Dadgar H, Ghareh-Aghaji N, Mohammadzadeh M 2014 J. Cancer Res. Ther. 10 896
 Google Scholar
Google Scholar
计量
- 文章访问数: 9930
- PDF下载量: 128
- 被引次数: 0












 下载:
下载: